Contents
- When Is Hormone Treatment Useful?
- When do doctors use hormone therapy for infertility?
- Female Infertility
- Hormone Treatment for Female Infertility
- Male Infertility
- Hormone Treatment for Male Infertility
- Why is that if testosterone is necessary for spermatogenesis (sperm cell maturation)?
- How Does Hormone Treatment Work?
For couples trying to conceive, Trusted sourceInfertility: Symptoms, Treatment, DiagnosisUCLA HealthGo to sourceinfertility can put their hopes and dreams into a painful reality filled with questions, treatments, and exorbitant costs. The options can be confusing, scary, and expensive. However, for some couples, the use of affordable hormone therapy for infertility can be the answer they seek.
Although not every woman or man is a candidate for hormone replacement therapy for infertility, many are. HRT should be one of the first options discussed as it can sometimes speed up the ability to conceive and save a significant amount of money. Do not hesitate to get a second medical opinion before trying more costly and invasive procedures.
Most people naturally associate hormone therapy with women. Hormone treatments are also used when in vitro fertilization is necessary. There is significantly less research to date on male hormone therapy for infertility and conception. Yet, according to research, infertility in males is the sole reason for the inability to conceive for at least twenty percent of couples. In many of these instances, there is no identifiable cause of male infertility, often complicating treatment options.
In this report, we look at the following subject matter:
- When hormone treatment is useful for conception
- Female infertility causes, signs, symptoms, and diagnosis
- Hormone therapy options for female infertility
- Male infertility causes, signs, symptoms, and diagnosis
- Hormone therapy options for male infertility
- How hormone treatment works for infertility
Infertility is an often painful topic for many couples. Hormone therapy may be useful as a tool to aid conception.
When Is Hormone Treatment Useful?
As we age, the body goes through many physiological changes. Hormonal decline and imbalance are natural occurrences that can cause physical, mental, and emotional problems for some people. Unfortunately, Trusted sourceEverything You Should Know About Hormonal ImbalanceHealthlineGo to sourcehormonal imbalance in males and females can also affect fertility. When that occurs, the use of hormone therapy for fertility problems can lead to a viable pregnancy.
When do doctors use hormone therapy for infertility?
Hormone therapy is beneficial when a lack of conception is caused by hormonal imbalance. If a man has low testosterone levels, he will likely suffer from a reduced sperm count. There are hormone therapies that can help stimulate natural testosterone production, as we will discuss further down this page. For a woman, hormone treatment can help when there are problems with egg maturation and ovulation. We will delve further into this in the next two sections.
In addition to the use of sex hormones such as progesterone, testosterone, and estrogen that we will discuss in-depth, there are other hormones to consider when dealing with infertility, including:
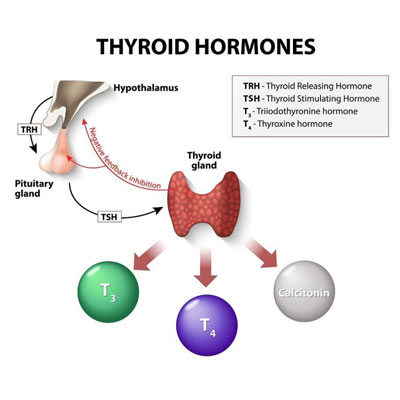
- Thyroid hormones
- Growth hormones (HGH)
- Follicle-stimulating hormone (FSH)
- Luteinizing hormone (LH)
- Prolactin
- Human chorionic gonadotropin (HCG)
Hormone therapy for infertility may not be helpful if the following causes are present:
In males
- Alcohol, tobacco, or drug use and abuse
- Undescended testicles
- Diabetes
- Injury, trauma, or tumor to the testicles
- Sperm blockage in the vas deferens
- Steroid use or abuse
- Use of sauna, hot tubs, or overly tight underwear
- Chemical, xenoestrogen, and phytoestrogen exposure
- Mumps virus
- Erectile dysfunction resulting in premature or lack of ejaculation
- Certain genetic diseases or DNA damage
- Depression causing low libido
- Stress
In females
Structural abnormalities such as:
- Uterine growths such as fibroids or polyps
- Endometriosis
- Abnormal cervical or uterus anatomy
- Uterine scar tissue
- Blocked fallopian tubes
- Pelvic inflammatory disease (PID) caused by gonorrhea or chlamydia
- Fallopian tube damage from pelvic infections of prior surgery
- Reduced egg supply
- Steroid use and abuse
- Athletic overtraining
- Stress
- Celiac disease
- Diabetes
- Sickle cell disease
- Kidney disease
- Some medications
- Chemical, xenoestrogen, and phytoestrogen exposure
- Drug, alcohol, or tobacco use
Hormone therapy for infertility is beneficial when the cause of the problems is a hormonal imbalance.
Female Infertility
The most common use of hormone therapy for fertility occurs in women. Problems with infertility can occur at many points along the axis, often due in nature to some form of hormonal issue.
The problem could originate in the hypothalamus, pituitary gland, thyroid gland, ovary, follicles, fallopian tube, or uterus.
Many of the non-hormonal causes of female infertility were discussed in the previous section.
The lists below outline causes that are more hormonal based, as well as signs and symptoms, and diagnostic methods:
Causes
- Polycystic ovarian syndrome (PCOS) – increased egg follicles on the ovaries affecting single follicle maturation (high testosterone levels are often present)
- Not enough follicle-stimulating hormone – lack of FSH reduces follicle and egg maturation
- Low levels of luteinizing hormone – not enough LH inhibits ovulation
- Too much prolactin – increases mammary gland growth and suppresses ovulation
- Low thyroid hormone levels – hypothyroidism (low levels) can interfere with female fertility when the thyroid gland does not produce enough thyroid hormones
- Growth hormone deficiency – aside from pituitary GH, the ovaries produces some growth hormone that aids in monofollicular growth
- Progesterone deficiency – progesterone is the “pregnancy hormone” that helps prepare the uterus for implantation of the fertilized egg, and low progesterone levels can inhibit implantation
- Primary ovarian insufficiency (POI) – a rare cause of infertility in women that brings early menopausal symptoms, absent or irregular periods, and other issues
Signs and Symptoms
- Irregular periods
- Absent periods
- Heavy or painful periods
- Hormonal imbalance symptoms
- Painful intercourse
Diagnosis
Diagnosing infertility often encompasses several steps besides a physical examination and medical history review, including:
- Ultrasound – to monitor ovarian follicular growth and ovulation as well as uterine issues
- Blood tests – to measure hormone levels
- Hysterosalpingography – an X-ray with contrast injected into the uterus helps determine uterine abnormalities
- Ovarian reserve testing (imaging and blood) – checks the quantity and quality of a woman’s eggs
The use of hormone therapy for infertility depends on what the testing shows. If hormonal problems are present, even in conjunction with other issues, the doctor may prescribe the appropriate hormone treatment to address the situation.
Female infertility can stem from hormonal imbalance, structural problems, or other issues that a doctor can diagnose through various testing mechanisms.
Hormone Treatment for Female Infertility
Many hormones can help with female infertility. ART is the abbreviation for assisted reproductive technologies, that encompasses various treatments that address infertility. The type of hormone treatment depends on the issue present. Some hormones support ovulation; others support follicular development.
Hormone therapy for infertility typically begins between day three and five after the start of menstruation. Depending on the treatment prescribed, it can be oral or injectable. Of course, the type of hormone therapy dictates when, how often, how much, and how long the treatment must continue. Each woman will discuss her options with her fertility doctor to select the path most suited to her needs.
Options for female hormone fertility treatments include:
- Progesterone – may be used vaginally or as an injection to help prepare the uterus for conception by thickening the endometrium. Progesterone hormone therapy for infertility is also crucial for nurturing the developing fetus.
- Estrogen – a crucial treatment for women with POI who will not respond to traditional hormones for infertility. Estrogen therapy may help ovarian follicles avoid premature luteinization. Doctors often prescribe a pre-treatment with estradiol before treating with gonadotropins to support follicular maturation and ovulation. Doctors may also prescribe estrogen during an IVF cycle, along with progesterone to help thicken the uterine lining.
- Thyroid hormones – hypothyroidism can inhibit ovulation, preventing conception. Measuring thyroid hormone levels, along with other hormones, is crucial to determine if thyroid hormone treatment is necessary. Women with hypothyroidism need to bring their thyroid levels into balance to improve the odds of conception.
- Human growth hormones – the use of growth hormone for infertility is beneficial to help increase ovarian sensitivity to gonadotropin stimulation.
Other benefits of HGH infertility treatment include:
- Enhancing aromatase to support testosterone conversion to estradiol to improve follicle and gamete maturation
- Inhibiting follicle apoptosis (death) along with gonadotropins to promote follicular survival (strengthening luteinizing hormone action)
- Improving oocyte maturation and fertility (beneficial for harvesting and in vitro fertilization)
- Follicle-stimulating hormone – FSH injections are beneficial when improved follicular and ova development is necessary.
- Human menopausal gonadotropin – a combination of FSH and LH injections to stimulate ova maturation and improve ovulation.
- Human chorionic gonadotropin – the use of injectable HCG can help egg maturation and trigger ovulation – often within 36 hours.
- Clomiphene – an anti-estrogen oral medication that tricks the body into thinking estrogen levels are low, prompting the pituitary gland to increase the production of LH and FSH for improved follicular development if ovulation is a problem. It is used for no more than six menstrual cycles before turning to other methods.
- Letrozole – not as commonly used, this medication taken for five days may help promote ovulation. Letrozole may work better for PCOS than clomiphene.
- Gonadotropins – injections of certain medications for seven to ten days can bypass the pituitary gland and help stimulate multiple egg production in the ovaries (beneficial for in vitro fertilization). Gonadotropins may increase multiple births.
- Metformin – beneficial for women when PCOS or insulin resistance are interfering with conception to improve insulin resistance to support ovulation.
- Bromocriptine – an oral dopamine agonist that is prescribed when excess prolactin production by the pituitary gland inhibits ovulation.
Follicular development can be checked with ultrasound and blood tests eight days after the menstrual cycle to determine the efficacy of the hormone treatment. Spontaneous ovulation often occurs once the largest follicle reaches 18 to 20 mm in size. If ovulation does not occur naturally, HCG can help trigger the egg release.
Doctors have many types of hormone therapy available to help with female infertility depending on the problems preventing conception.
Male Infertility
Although not as common as with females, males can also have hormonal imbalances that affect fertility. We previously discussed the causes of male infertility that are not due to hormones earlier in this report. As with women, problems with infertility can occur in many locations along the hypothalamic-pituitary-gonadal axis.
Before beginning any form of hormone replacement therapy for male infertility, the doctor will run several tests to try and determine the cause of any fertility issues. Physical examination and a discussion of lifestyle habits and medical history are also part of the diagnostic process.
Here are the lists of hormonal causes, signs and symptoms, and diagnostic tools to check for male infertility:
Causes
- Not enough luteinizing hormone – decreases signals to the Leydig cells in the testes to produce testosterone
- Low levels of follicle-stimulating hormone – inhibits spermatogenesis when not enough FSH is present
- Testosterone deficiency – testosterone is necessary to support spermatogenesis
- Growth hormone deficiency – growth hormone also aids in sperm maturation, as well as helping stimulate testosterone production as some GH is expressed in the testes
- Elevated thyroid hormone levels (rare condition) – hyperthyroidism may result in abnormal sperm motility and may damage spermatozoa
- Low thyroid hormone levels (rare condition) – hypothyroidism may cause abnormal sperm morphology as well as decreases in testosterone, LH, and FSH levels
Signs and Symptoms
- Testicular pain or swelling
- Changes in libido
- Erectile dysfunction – inability to maintain an erection
- Testicular shrinkage
- Ejaculatory problems
Diagnosis
- Semen analysis – checks for abnormalities in shape, motility, infections, and sperm count
- Hormone testing – to check hormone levels for deficiency
- Scrotal ultrasound – determines if there are problems in the testicles or supporting structures
- Genetic testing – may be performed with extremely low sperm count to detect any genetic abnormality
- Post-ejaculation urinalysis – to detect if sperm are traveling back into the bladder rather than out of the penis during ejaculation
- Testicular biopsy – may help determine a blockage
- Transrectal ultrasound – checks the prostate and determines if blockages of the ejaculatory ducts or seminal vesicles are present
Hormone therapy for infertility in males can help improve conception outcomes.
Hormone Treatment for Male Infertility
The use of hormone therapy for infertility in males is commonplace today when hormonal imbalances are present. What may surprise you to know is that if a man has a testosterone deficiency, the doctor will NOT prescribe testosterone replacement therapy. The use of testosterone for male infertility will only worsen the problem, not improve it.
Why is that if testosterone is necessary for spermatogenesis (sperm cell maturation)?
Only testosterone produced in the testes can work locally on sperm cells. When testosterone enters the body through supplemental methods, that testosterone stays in the bloodstream and cannot enter the testes. With the hypothalamus sensing higher levels of testosterone in the body, testicular testosterone production may decrease, often worsening infertility. That is why doctors do not prescribe testosterone therapy for infertility.
It is also rare for men to be diagnosed with hyperthyroidism. If that should occur, you will speak with an endocrinologist to discuss possible treatment options of lowering thyroid hormone levels depending on the cause.
Here are the most common options of hormone therapy for infertility in males:
- Human chorionic gonadotropin – for men with hypogonadotropic hypogonadism (HH), HCG works in the same way as LH, stimulating the Leydig cells to increase testosterone production. HCG is also used in conjunction with testosterone therapy in men with Low T to prevent testicular atrophy and maintain testosterone production.
- Human menopausal gonadotropin and HCG – together, these hormone therapies increase spermatogenesis more than either medication alone. Pre-treatment testicular volume determines which treatment to use.
- Follicle-stimulating hormone – some men may benefit from FSH therapy to increase sperm maturation.
- Luteinizing hormone – doctors typically try HCG before using a combination of LH and FSH to promote fertility.
- Clomiphene – binds to hypothalamus estrogen receptors to increase signals to the pituitary gland to promote LH and FSH secretion. Increased LH tells the Leydig cells in the testes to produce testosterone. FSH promotes sperm cell maturation.
- Aromatase inhibitors – AIs help block the conversion of testosterone into estrogen, leaving more testosterone in the body to promote spermatogenesis. Studies have shown AIs to help increase LH, FSH, and testosterone levels.
- Human growth hormone – both HGH and insulin growth factor 1 (IGF-1) exhibit gonadotropic effects that aid in testosterone production and/or spermatogenesis. HGH acts at the testicular levels in both autocrine and paracrine ways to improve testosterone levels and sperm maturation. The use of HGH for male infertility may help increase sperm concentration and motility.
- Thyroid hormone – if hypothyroidism is diagnosed, then treatment with thyroid hormone (T4) is necessary to improve thyroid, LH, FSH, and testosterone levels. T4 treatment can help improve sperm motility and morphology.
Depending on the hormonal imbalance, numerous options in hormone replacement can help improve male fertility.
How Does Hormone Treatment Work?
The use of hormone therapy for infertility in men and women requires proper diagnostic testing and medical supervision. A fertility or hormone specialist is necessary for any treatment in this area. Fertility is a complicated issue, and a specialist will look at all potential causes of conception difficulties before embarking on a course of treatment.
Hormone therapy helps to put the necessary hormone levels back in proper balance so that the body can function properly.
Infertility often affects a couple emotionally, as well as physically and even financially. Some treatment options, such as IVF, are expensive – and there is no guarantee that they will work. Hormone treatments can also affect a person’s emotional state, especially for women who have to use daily hormone shots. For some couples, getting off of hormone therapy for infertility may be necessary after a few months if the treatments are not providing the desired results. Luckily, doctors have many options available today to try if others do not work.
Do not despair if you or your partner are diagnosed with infertility. There are many avenues of treatment to discuss. If you are currently on some type of hormone treatment and thinking about stopping hormone therapy for infertility since you have not yet become pregnant, do not hesitate to contact HGH Doctor for more information about this topic. We are happy to help you understand the options available to you.
- Amr Ismail El Meliegy, MD, Ahmad Motawi, MSc., MD, FECSM, Mohamed Ahmed Abd El Salam, Msc ,MD
- Darshan Prahlad Patel, MD, William O. Brant, MD, FACS, FECSM, Jeremy B. Myers, MD, Angela Presson, PhD, MS, Erica Boiman Johnstone, MD, MHS, J. Dorais, Kenneth I. Aston, PhD, Douglas T. Carrell, PhD, HCLD, James M. Hotaling, MD, MS, FECSM
- Dr. Ronald Wiehle, PhD, Greg Fontenot, PhD, Jennifer L Wike, Kuang Hsu, Jennifer Nydell, Larry I Lipshultz, MD
- M. Monastirska, K. Tsvetkov, A Simeonova, R. Murad, E. Zheleva
- Peter Y Liu, David J Handelsman
Systematic review of hormone replacement therapy in the infertile man.
The safety and efficacy of clomiphene citrate in hypoandrogenic and subfertile men
Enclomiphene citrate stimulates testosterone production while preventing oligospermia: A randomized phase II clinical trial comparing topical testosterone.
Hormone replacement therapy at women with fertility problems and proofs of hypergonadotropic hypoovarism
The present and future state of hormonal treatment for male infertility