Contents
- What Is Thyrotropin Hormone?
- What is thyrotropin hormone function, and why is it important?
- What Regulates Thyrotropin Hormone?
- What Happens If Thyrotropin Hormone Levels Are Low?
- What Happens If Thyrotropin Hormone Levels Are Too High?
- How Do You Test Thyrotropin Hormone?
- How Do You Balance Thyrotropin Hormone?
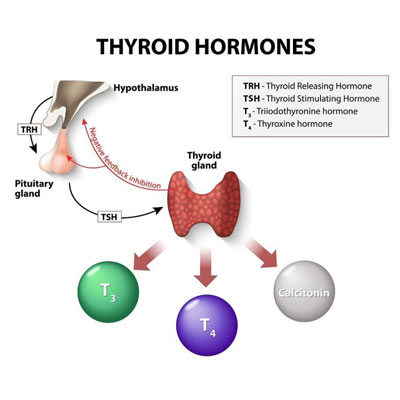
As with many hormones, Trusted sourceThyrotropin-releasing hormoneYou and Your HormonesGo to sourcethyrotropin hormone also goes by a variety of names, including thyrotropic hormone, thyrotrophin, and thyroid-stimulating hormone or TSH. Thyrotropin is a glycoprotein hormone discovered by Bennet M. Allen and Philip E. Smith in 1916. That is when they found that the pituitary gland contained a thyrotropic substance.
The definition of thyrotropin is a hormone secreted by the anterior pituitary gland to regulate the production of thyroid hormones. In this role, TSH plays a crucial function as thyroid hormones stimulate the metabolism of most of the body’s tissues.
Unlike many hormones that remain in the bloodstream all day, thyrotropin hormone has a half-life of only about an hour. After that, only half of the secreted TSH is left in circulation.
In this report, we will cover the following information about thyrotropin:
- The function of thyrotropin hormone
- How thyrotropin production is regulated
- What happens when thyrotropin hormone levels are low
- What happens when thyrotropin hormone levels are too high
- How to test TSH levels
- How to balance thyroid-stimulating hormone levels
Thyrotropin hormone secreted by the pituitary gland stimulates the release of thyroid hormones into the bloodstream.
What Is Thyrotropin Hormone?
Thyrotropin hormone is composed of two subunits non-covalently bound to each other. That means they do not share a pair of electrons.
Thyrotropin’s alpha subunit is present in human chorionic gonadotropin (HCG), luteinizing hormone (LH), and follicle-stimulating hormone (FSH), as well. The beta subunit is unique to thyrotropin. The alpha subunit has a 92 amino acid sequence, and the beta subunit has a 118 amino acid sequence.
When attached, the alpha and beta subunits can bind only to thyrotropin-stimulating hormone receptors. Unbound, the alpha and beta subunits provide no biological activity.
What is thyrotropin hormone function, and why is it important?
Without TSH, the thyroid gland could not secret its two hormones – Trusted sourceThyroxine OverviewHormone Health NetworkGo to sourcethyroxine (T4) and Trusted sourceTriiodothyronine You and Your HormonesGo to sourcetriiodothyronine (T3).
Together, these two thyroid hormones help regulate the following functions:
- Brain development
- Long bone growth
- Muscle control
- Digestion
- Heart functions
- Metabolic rate (T4)
- Protein synthesis
- Sensitivity to catecholamines (adrenaline)
- Protein, carbohydrate, and fat metabolism
- Vitamin metabolism
As we look at the uses of thyrotropic hormone, it helps to understand the functions of T3 and T4. Thyroxine is the precursor hormone to triiodothyronine. T4 is the primary form of thyroid hormone, lasting longer than T3, having a ratio of 14:1. Once T4 converts into T3, triiodothyronine is three to four time more potent than thyroxine.
Thyrotropin hormone stimulates the release of thyroid hormones from the thyroid gland.
What Regulates Thyrotropin Hormone?

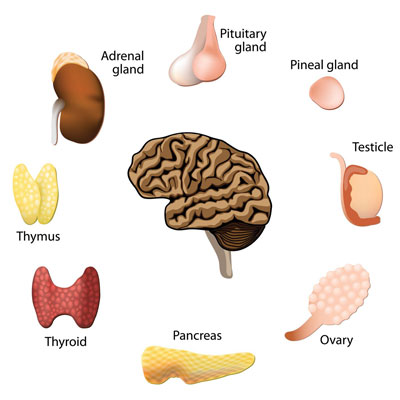
Upon receipt of thyrotropin-releasing hormone, normal actions take place in the pituitary gland to secrete TSH into the bloodstream. Once thyrotropin-stimulating hormone enters the circulation, it heads to the thyroid to promote T3 and T4 production. Upon reaching the thyroid, thyrotropin hormone finds its receptors on thyroid follicular cells.
TRH lasts only two minutes as its distance from the hypothalamus to the pituitary gland is less than an inch. As soon as it enters the pituitary gland, it is broken down and utilized for TSH production.
Now, if the hypothalamus senses too much thyroid hormone in the bloodstream, it will not release TRH to the pituitary gland. Instead, it will send a supply of somatostatin to decrease or inhibit its release. We should also point out that somatostatin inhibits growth hormone production, as well.
Because HCG has some cross-reactivity to TSH receptors, it can stimulate some thyroid hormone production. If a woman continues to have high concentrations of HCG during pregnancy, she could experience a condition called gestational hyperthyroidism.
The hypothalamus secretes a thyrotropin-releasing hormone to the pituitary gland to stimulate thyrotropin hormone production.
What Happens If Thyrotropin Hormone Levels Are Low?
If you have low thyrotropin hormone levels, you could have an overactive thyroid or hyperthyroidism.
Causes of low TSH levels include:
- Too much iodine
- Taking a supplement that contains thyroid hormone causing TSH levels to decline
- Graves’ disease – the immune system begins to attack the thyroid gland
- Taking too high a dosage of thyroid hormone
Some medications and supplements can lower TSH levels, causing false readings, including:
- Dopamine
- Opioids
- Steroids
- Biotin
Low thyrotropin-stimulating hormone levels occur because the hypothalamus senses that the bloodstream contains too much T3 and T4, causing it to send somatostatin to the pituitary gland. That reduces the amount of TSH sent to the thyroid gland. When thyrotropin hormone release declines in this scenario, the following symptoms from hyperthyroidism are possible:
- Weight loss
- Anxiety
- Heart palpitations
- Feeling hot
If both TSH and thyroid hormone levels are low, it can signal secondary or “central” hypothyroidism. Secondary hypothyroidism typically occurs due to insufficient TRH release from the hypothalamus of decreased TSH production from the pituitary gland.
When TSH levels are low, but thyroid hormone levels are high, it can mean primary hyperthyroidism in the form of Graves’ disease.
Low thyrotropin hormone levels could indicate an overactive thyroid.
What Happens If Thyrotropin Hormone Levels Are Too High?
Elevated TSH levels may signify an underactive thyroid. When that happens, the thyroid does not respond to the signals from TSH to produce thyroid hormones. The hypothalamus continues to sense low thyroid hormone levels and sends more TRH to the pituitary gland, which, in turn, sends even more thyrotropin hormone into the bloodstream.
An underactive thyroid gland is also called hypothyroidism and can cause a person to gain weight, feel cold, and become lethargic. In some cases, the thyroid gland may become enlarged, forming a goiter. Other symptoms are often associated with Hashimoto’s thyroiditis (see below) and may include constipation, general pains, thinning hair, heavy menstrual flow in women, pale or puffy face, and depression.
If both TSH and thyroid levels are high, the problem could be an adenoma (benign tumor) in the pituitary gland. Thyroid hormone resistance is another possibility.
If TSH levels are high, but thyroid hormone levels are low, the causes could be:
- Congenital hypothyroidism – a thyroid hormone deficiency present at birth that can cause growth failure and permanent intellectual disability (screening is done at birth)
- Primary hypothyroidism – may be caused by iodine deficiency or Hashimoto’s thyroiditis, radiation to the neck, lithium use, surgical removal of all or part of the thyroid gland
- Hashimoto’s thyroiditis – an autoimmune disease that occurs as the thyroid gland is gradually destroyed, a goiter may also occur
Elevated thyrotropin hormone function levels may signal an underactive thyroid gland.
How Do You Test Thyrotropin Hormone?
A TSH test is ordered to determine if your thyroid gland is working properly. The thyroid-stimulating hormone test can detect thyroid disorders even before any symptoms are present. It is important to detect a thyroid disorder as it could lead to further health problems if untreated.
Unlike many other blood hormone tests, the specimen collection can take place at any time of the day. Many other hormone tests are run first thing in the morning while fasting. Because your doctor will likely order other blood panels at the same time, you may still need to visit the lab early in the morning for this test. Fasting is not necessary unless required for other tests. Your doctor may want to check insulin growth factor 1 levels to detect if you are growth hormone deficient. That could occur if TSH levels are low due to somatostatin release caused by high thyroid hormone levels.
The doctor will likely order free T3, free T4, reverse T3, and an anti-TPO antibody test to determine if you require treatment for a thyroid disorder.
When testing for thyrotropin hormone, it is unlikely that you will need to stop taking any medications or supplements. However, you should still let your doctor know because certain drugs could alter thyroid function.
Normal TSH levels are between 0.4 and 4.0 mU/L, although some labs may consider up to 5 mU/L as normal. Anything higher could indicate an underactive thyroid gland.
Pregnant women often have higher T3 and T4 levels and lower TSH levels.
Blood analysis measures TSH and thyroid hormone levels.
How Do You Balance Thyrotropin Hormone?
If you have an underactive thyroid, the hormone doctor may prescribe a synthetic thyroid hormone pill that you will take each day. Benefits of improving thyroid levels include more energy and weight loss. Rechecking of TSH levels is typically done two to three months after the start of treatment. Increasing thyroid hormone with medical intervention helps to lower thyrotropin-stimulating hormone levels back to a normal range.
For people with an overactive thyroid, the doctor may decide on one of the following options:
- Anti-thyroid medications (pills) to reduce thyroid gland hormone production
- Beta blockers that lower a rapid heart rate that results from having high thyroid levels
- Radioactive iodine treatment to slow the thyroid
- Thyroidectomy – surgical removal of the thyroid (less common)
If you have hypothyroidism, it is best to avoid the following foods if you have iodine deficiency:
- Any soy products
- Nuts and seeds
- Sweet potatoes
- Peaches
- Strawberries
- Cassava
- Cabbage
- Spinach
- Kale
- Cauliflower
- Broccoli
- Millet
For hypothyroidism without iodine deficiency, it may be helpful to avoid or significantly reduce:
- Millet
- Gluten
- Processed foods like cookies, cakes, hot dogs, luncheon meats
- Cruciferous vegetables
- Pears, strawberries, peaches
- Soy-containing foods
- Coffee
- Green tea
- Alcohol
- Supplements zinc and selenium
If you have hyperthyroidism, it may help to avoid the following foods:
- Fish
- Shellfish
- Seaweed
- Carrageen (food additive)
- Iodized salt
- Some food colorings
- Egg yolks
- Cheese
- Milk and dairy
- Iodine-containing medications and supplements
- Nitrates in processed foods
- Gluten
- Soy
- Vegetables: spinach, cucumber, pumpkin, carrots, turnips, cabbage, beets, lettuce, parsley, leeks, endive, dill, celery
For additional information on thyrotropin hormone, or to speak with a medical advisor about any other hormone concerns, please contact HGH Doctor hormone clinic. We provide free, confidential consultations by phone to men and women throughout the US.
- Joshua Estrada, Dr. Timothy M. Buckey MD, Dr. Kenneth D., Burman, MD, Offie P Soldin, PhD
- Ulla Feldt-Rasmussen, MD, DMSc, Sofie Bliddal, Dr. Åse Krogh Rasmussen, Malene Boas, PhD, Linda Maria Hilsted. MD, DMSc, MPA, Katharina Maria Main
- Gil Atzmon, PhD, Nir Barzilai, MD, Dr. Joseph G. Hollowell, Martin Surks, MD
- William C. Shiel Jr., MD, FACP, FACR
- Author: Stephanie L Lee, MD, PhD; Chief Editor: Romesh Khardori, MD, PhD, FACP
- Ferdinand Roelfsema, Johannes D. Veldhuis
- Maria Izabel Chiamolera, Fredric E. Wondisford
Thyrotropin Isoforms: Implications for Thyrotropin Analysis and Clinical Practice
Challenges in Interpretation of Thyroid Function Tests in Pregnant Women with Autoimmune Thyroid Disease
Extreme Longevity Is Associated with Increased Serum Thyrotropin
Medical Definition of Thyrotropin
What is the role of thyrotropin-releasing hormone (TRH) in the pathogenesis of hyperthyroidism?
Thyrotropin Secretion Patterns in Health and Disease
Thyrotropin-Releasing Hormone and the Thyroid Hormone Feedback Mechanism