Contents
Exposure to stress during one’s early life can influence short-term or long-term effects on the development of the brain. Anxiety, depression, and learning deficits are possible. Stress can increase cortisol release from the adrenal cortex, affecting the hypothalamic-pituitary-adrenal axis. The result is altered or inhibited release of crucial hormones from the hypothalamus and pituitary gland.
Long-term elevated levels of corticosterone levels desensitize glucocorticoid and mineralocorticoid receptors, inhibiting efficient negative feedback in the HPA axis loop. Depression is often stress-related having to do with some form of a chronic or emotional situation. The stress associated with depression often includes changes in the levels of vital neurotransmitters in the brain, including dopamine, serotonin, noradrenaline, GABA, epinephrine, and glutamate. Dopamine decline is associated with PD.
When dopamine levels decline, prolactin levels often increase, which can adversely Trusted sourceProgesterone and Parkinson’s DiseaseNCBIGo to sourceimpact progesterone , testosterone, and estrogen levels, which we will examine further down in this report. Another aspect to consider is the increase in serotonin levels associated with stress that can hinder sleep and increase depression and emotional disorders. Lack of sleep interferes with the production of many hormones, including testosterone and growth hormone.
The hormones – Trusted sourceWhat Is Parkinson's?Parkinson`s FoundationGo to sourceParkinson's disease connection may also be linked to the fact that the gender ratio of men to women is about two to one. Does that mean that hormones may play a role in Parkinson’s development, and if so, can hormone therapy help reduce the risk? These are the questions we will examine in this report.
Worth examining is the connection between thyroid hormones and Parkinson’s. Free triiodothyronine hormone levels are often significantly lower in PD patients, which is associated with motor symptoms in de novo PD patients (not yet taking Parkinson’s medications). An overlapping of symptoms is often present with hypothyroidism and Parkinson’s, which is why testing of thyroid function and levels is important. Any patient diagnosed with PD should receive a complete hormone serum profile.
Numerous hormones may impact the development and progression of Parkinson’s disease.
What Is Parkinson’s Disease?
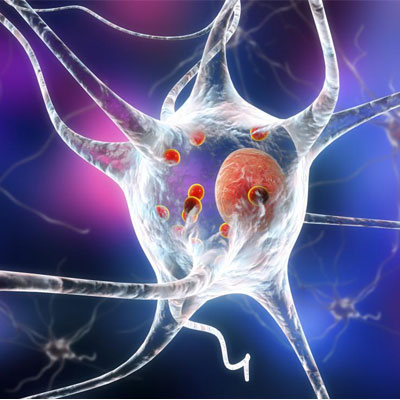
Parkinson’s disease (PD) is a slowly developing neurodegenerative disorder affecting the dopamine-producing neurons in the substantia nigra area of the brain. Complications resulting from Parkinson’s make it the 14th leading cause of death in the US. There is no definitive cause or cure for PD, which is typically associated with the following symptoms:
- Tremors mainly while at rest – often seen in the hands
- Limb rigidity – resistance to movement
- Bradykinesia – slow movement
- Hyperkinesia – reduced movement amplitude
- Akinesia – absence of normal unconscious movement
- Postural instability – problems with gait and balance
Parkinson’s disease is marked by progressive deterioration of nerve cells that produce dopamine in one part of the brain. Trusted sourceWhat Is Dopamine?Psychology TodatGo to sourceDopamine is a crucial chemical messenger (hormone) necessary for communication between the areas of the brain (basal ganglia) that help regulate nerve functions and smooth muscle movement. That is why speech, walking, and performance of daily tasks are often difficult for people with Parkinson’s.
The basal ganglia consist of nuclei made up of the substantia nigra, putamen, caudate nucleus, globus pallidus, and subthalamic nucleus that form an interconnecting network to process chemical signals that lead to movement actions and terminations.
Environmental toxin exposure may also trigger the neuronal death seen in Parkinson’s disease. Exposure to toxic substances can leave the brain vulnerable to chronic physiological stress.
Oxidative stress and neuroinflammation are also contributing factors, which can come from hormonal imbalances. One way that hormones may play a role in Parkinson’s development is when a person is deficient in growth hormone, which also leads to a decline in insulin growth factor 1. HGH and IGF-1 are crucial for neurogenesis and provide neuroprotective benefits for the brain and central nervous system.
Parkinson’s disease is a slowly developing neurodegenerative disorder marked by progressive nerve cell deterioration, tremors, and decline in movement.
Female Hormones and Parkinson’s disease
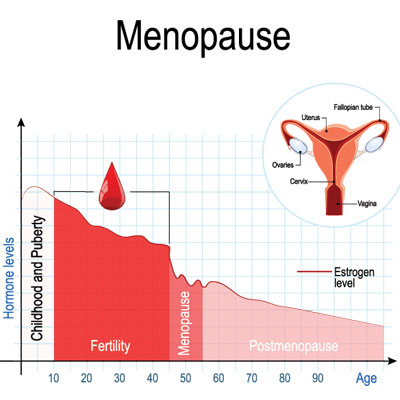
Women may have an advantage when it comes to developing Parkinson’s disease – especially if they were fertile for over 39 years and went through natural menopause. However, according to one study, those females who had four or more pregnancies have a greater risk of developing Parkinson’s.
In this section, we look at how hormones may play a role in Parkinson’s development in females. A woman’s fertile life span encompasses the years between the first menstrual period and the time of menopause. According to Rachel Saunders-Pullman, MD, MPH, a leading neurology specialist from Albert Einstein College of Medicine and Beth Israel Medical Center in New York City, the average span is about 35 or 36 years for most women.
Increased lifetime estrogen exposure may be the reason women are less at risk of developing PD than men. Progesterone is also believed to have neuroprotective benefits for Parkinson’s. It is a natural anti-inflammatory that doctors even use to treat traumatic brain injury and stroke as it protects the myelin (outer nerve sheaths). Progesterone production occurs inside the brain and throughout the nerves in the spinal cord so that it can act directly in those areas.
After examining research from the Women’s Health Initiative Study (WHI), Dr. Saunders-Pullman and her colleagues gathered the following findings about hormones and Parkinson’s disease:
- Women who reported four or more pregnancies along with natural menopause had a 20% increased Parkinson’s disease risk as compared to those with three or fewer pregnancies. There was no increase in risk for higher pregnancies and surgical menopause.
- Females whose fertile life span lasted 39 or more years who also had natural menopause had an 18% reduction in Parkinson’s risk compared to women with less than 33 years. There was no link found between surgical menopause and fertile life span.
- Women who experienced surgical menopause and had also used prior hormone replacement therapy were at double the risk when compared to non-users of HRT. Females currently using HRT experienced no increased risk when compared to those who had never used hormone therapy.
- Women who used HRT and underwent natural menopause also did not have an increased risk of developing Parkinson’s compared to those who never used hormone therapy. There was also no difference in current vs. never-users.
Fertile life span in women can impact the risk of Parkinson’s disease.
Pregnancy, Hormones, and Parkinson’s
We do not know why pregnancy number increases the risk, but speculation of declining hormone levels during multiple postpartum periods may shed light on how female hormones may play a role in Parkinson’s. The thought process is that estradiol helps decrease PD risk, but overexposure to estriol (the primary form of estrogen during pregnancy) can increase it in women with four or more pregnancies.
There is one other issue to discuss about pregnancy and Parkinson’s, and that is women becoming pregnant when they have PD. Few cases of this exist due to most women who develop PD doing so long after menopause, and one of the primary concerns is that of birth defect risk associated with antiparkinson’s medications. Dopamine agonists are considered safe, but they block milk production, making it impossible for a woman to breastfeed. Other medications may cause problems, so it is vital to discuss this with your doctor. PD does not affect female fertility, but it can cause self-image issues that impact libido.
Parkinson’s motor and non-motor symptoms may increase during pregnancy, although not to the point where they impact overall functioning. Following delivery, non-motor symptoms tend to improve. However, any progression in movement, tremors, or rigidity tends to persist.
Pregnancy is possible for younger women with Parkinson’s disease, but it is crucial to discuss treatment options with your doctor.
Male Hormones and Parkinson’s
Just as with females, males may also have symptoms of testosterone deficiency that resemble non-motor PD symptoms. Because hormones may play a role in Parkinson’s, all patients diagnosed with Parkinson’s disease should be tested for hormonal imbalance, including testosterone deficiency. Some of the PD symptoms labeled as non-motor parkinsonian manifestations could be due to Low T, and better treated with testosterone replacement therapy (TRT).
Symptoms often labeled as non-motor PD manifestations may include:
- Anxiety
- Fatigue
- Sexual dysfunction
- Depression
- Low libido
- Reduced quality of life
Antidepressant therapy used to treat some people with PD may not address these issues the way that using testosterone hormone for Parkinson’s disease might accomplish. Testosterone deficiency is often a co-morbidity in male patients with PD, which is why testing is crucial.
In one study of mice, castration causing a sudden decline in testosterone levels resulting in Parkinson’s-like symptoms and pathology. Testosterone supplementation provided to the male mice resulted in a reversal of the PD symptoms.
As a side note, caffeine intake is also associated with a decreased risk of PD in men.
Many men with Parkinson’s are also testosterone deficient.
Can Hormones Help Parkinson’s?
There may be various hormonal pathways for addressing Parkinson’s disease, both before onset and after. For people with depression, finding the right treatment as soon as possible is crucial. It may be possible to delay the development of neurodegenerative diseases such as PD by reducing chronic stress and depression. Testosterone, long the treatment of choice before the invention of antidepressants, is once again being used for people who do not respond to more conventional medications. However, hormone specialists believe in checking hormone levels before administering antidepressant medications. For many people, balancing their hormone levels can reverse emotional instability and depression, potentially reducing the brain damage that can lead to PD. Both testosterone and HGH therapy can reverse feelings of depression in those with corresponding deficiencies.
We earlier discussed the impact of stress and elevated levels of cortisol on Parkinson’s disease. What may seem to be counter to that discussion is a 2017 study that looked at using cortisol to prevent dopaminergic neurons from dying. In the study, cortisol was shown to stimulate parkin expression that provided a neuroprotective effect for the brain. Parkin protein mutations may contribute to movement problems and tremors. Stimulating parkin expression may offer protection against cellular stress and dopamine loss. However, low dose treatment would be necessary to prevent side effects including opposing testosterone and growth hormone levels, increasing blood pressure and blood glucose levels, and increasing the risk of the mental disorder psychosis that could damage the brain. As with all potential treatment options, it is essential to get a complete blood hormone workup before starting any therapy.
As we look closely at Parkinson’s hormone replacement therapy, we find benefits in the following ways:
- Progesterone – natural anti-inflammatory benefits to help maintain neuronal tissue operations, regulates synaptic functions, and supports neurotransmitters
- Estrogen – more research is necessary as to the benefits of estrogen therapy for PD as it may have some merit during menopause for decreasing risks
- Testosterone – low levels of testosterone are often seen in men with PD and testosterone therapy can help reduce and reverse testosterone deficiency symptoms
- Human Growth Hormone – HGH stimulates the liver to secrete insulin growth factor 1, the essential mediator of many growth hormone functions for cell regeneration and brain health
Bioidentical hormones may play a role in Parkinson’s treatment by supporting healthy brain functions, reducing inflammation, improving fitness and exercise capability, decreasing tremors, and enhancing mobility. Balanced hormone levels also decrease mood changes and depression, supporting endorphin release.
- Office of Communications and Public Liaison., National Institute of Neurological Disorders and Stroke., Bethesda, MD., National Institute on Neurological Disorders and Stroke., National Institutes of Health.
- Connie Marras, MD., PhD., Rachel Saunders-Pullman, MD., MPH.
- Peifu Wang, Jilai Li., PhD., Shi Qiu, Honfeng Wen, Jichen Du.
- Louise Chang, MD.
- Society for Neuroscience
- Richelin V. Dye, PhD., Karen J. Miller, PhD., Elyse J. Singer, MD., Andrew J. Levine, PhD.
Parkinson’s Disease: Hope Through Research
The Complexities of Hormonal Influences and Risk of Parkinson’s Disease
Hormone replacement therapy and Parkinson’s disease risk in women: a meta-analysis of 14 observational studies
Hormones May Play a Role in Parkinson’s
Estrogen improves Parkinson’s disease symptoms
Neuroprotection and Neuroregeneration in Alzheimer’s Disease