Contents
- Stages of Menopause and Benefits of Hormone Therapy for Each One
- Types of Menopause Hormone Therapy
- Benefits of Hormone Therapy for Menopause
- Risks and Side Effects of Hormone Therapy
- Measuring the Pros and Cons of Hormone Therapy for Menopause
- The most important question to ask is, do the benefits outweigh the risks?
- How to Select the Right Type of Hormone Therapy
Hot flashes, mood swings, and mental fog may reduce work productivity and cause tension in personal relationships. Weak bones and hormonal influence on heart health and brain functions can lead to potential issues down the road.
These are only some of the reasons why a consultation with a hormone specialist about the prospective use of hormone replacement therapy (HRT) can benefit a woman.
A diagnosis of menopause is typically symptom-based.There is no menopause blood test or scan.
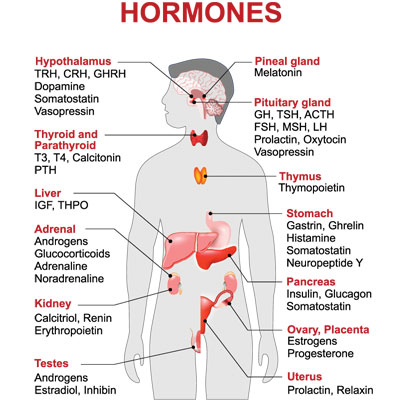
There is a blood test that can be measured to Trusted sourceFDA Approves Blood Test for MenopauseLab Tests OnlineGo to sourcediagnose menopause if the diagnosis is in question. It is follicle-stimulating hormone (FSH) and is produced in the pituitary gland located in the brain. As estrogen production and release decrease from the ovary, the lower blood levels trigger the pituitary to release more FSH. The purpose of FSH is to tell the ovaries to release more estrogen, but since the ovaries are failing, they cannot do that anymore. However, your doctor should run a comprehensive set of blood panels before putting you on any hormone therapy. There are many types of HRT, and the right treatment will focus on your specific needs and deficiencies.
As we explore what you need to know about HRT for menopause, we will look at the following:
- The three stages of menopause and the HRT benefits of each one
- Types of menopause hormone treatment
- Benefits of HRT
- Hormone therapy risks
- How to measure the pros against the cons
- How to select the right HRT option for you
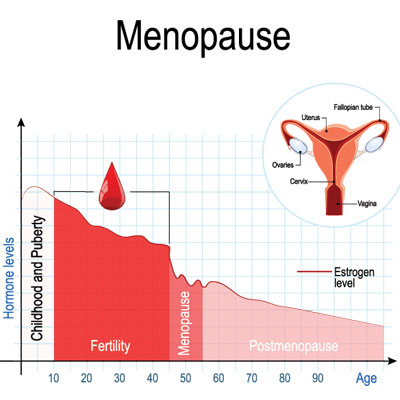
The average age for women to begin menopause in the US is approximately 51 years. Hormone replacement therapy focuses on each woman’s needs.
Stages of Menopause and Benefits of Hormone Therapy for Each One
Although the average onset of menopause is 51, 95% of women start to notice their changes occurring between 45 and 55 years of age. Menopause commences once the ovaries begin to decrease the production of critical hormones. Progesterone, testosterone, and estrogen are the primary hormones secreted by the ovaries. The adrenal glands, brain, and other tissues manufacture a small amount of these hormones. However, that is not usually enough to continue to carry out their functions. Depending on the stage of menopause, and the symptoms, the doctor will determine if HRT for menopause is necessary or beneficial.
The three stages of menopause are:
- Perimenopause – begins at the onset of the first symptoms and ends one year after the last menstrual period when the diagnosis of menopause is made. The monthly cycle becomes irregular, with changing gaps between periods. A woman can still become pregnant when in the perimenopause. The use of oral contraceptives may be needed to avoid pregnancy and manage irregular periods. because hormone therapy during this stage does not prevent pregnancy. The risk of mood changes is highest in this stage.
- Menopause – verified after the passing of twelve months without a period. The ovaries cease egg production. Symptoms of menopause are most likely to become bothersome. Hormone therapy to treat menopause can help protect the bones, brain, vaginal health and lubrication, heart, and overall health while also reducing unpleasant symptoms.
- Postmenopause – the remaining years after menopause when symptoms start to subside and disappear. The use of hormone therapy for menopause treatment later is typically symptom-specific. The goal of HRT is to administer the lowest dosage for the shortest time.
The three stages of menopause are perimenopause, menopause and postmenopause.
Types of Menopause Hormone Therapy
Although many doctors will say there are primarily two types of HRT for menopause, a hormone specialist may offer other alternatives.
The two primary types of hormone therapy for menopause treatment are:
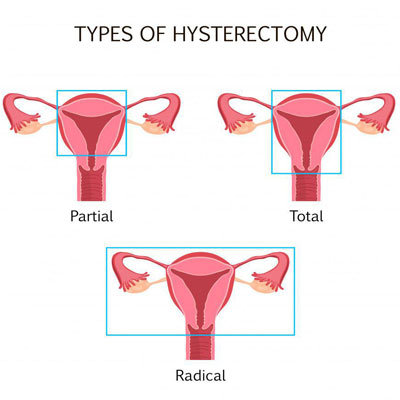
- Estrogen therapy (ET) – estrogen is the most prescribed type of HRT for menopause. It provides the relief of symptoms while helping to strengthen bones. ET by itself is the treatment typically given to females who have undergone a hysterectomy especially if the ovaries were removed at the same time.
- Estrogen combined with progesterone therapy (EPT) – estrogen and progesterone together are necessary when a woman still has her uterus. The reason is that estrogen alone could lead to endometrial cancer due to tissue overgrowth. Be careful only to use natural progesterone and not synthetic progestin as that can increase certain side effects risks.
The standard ET and EPT options include patches, pills, vaginal rings, gels, sprays, vaginal creams, or tablets. Doctors prescribe vaginal HRT to treat local symptoms only, such as vaginal wall thinning (atrophy), vaginal dryness, or urinary issues related to menopause.
Other treatment options to consider include bio-identical HRT for menopause:
- Natural progesterone – because the body uses progesterone to produce testosterone and estrogen, bioidentical progesterone therapy is a natural and safe way to increase these hormone levels.
- Testosterone – is formed from androstenedione in fat tissues which also gets converted to estrone, a weak form of estrogen. Testosterone replacement therapy is even considered safe for women who are unable to receive ET.
- Human growth hormone – the symptoms of growth hormone deficiency mimic much of what a woman experiences with menopause. GH levels begin to decline around age 30. Treating growth hormone deficiency with HGH therapy typically reveres the symptoms of menopause along with many other concerns.
A woman has options beyond estrogen or estrogen and progesterone to treat menopause symptoms.
Benefits of Hormone Therapy for Menopause
Before we discuss the benefits of HRT for menopause, we want to explain that not every woman will need hormone replacement therapy. If no current symptoms of menopause exist, or if they are mild in nature, life can often proceed without intervention. The purpose of HRT is to reduce the bothersome symptoms of menopause.
The benefits that stem from hormone therapy for menopause treatment include:
- Reversal or cessation of hot flashes and night sweats
- Improved sleep with fewer disturbances
- Improvement in vaginal issues such as atrophy, wall thinning, and dryness
- Enhanced sexual desire and pleasure
- Possibly beneficial effect on weight
- Bone strengthening
- Sharper mental functions and focus
- Better mood and improved quality of life
There was a time when ET or EPT was recommended for the treatment or prevention of osteoporosis and chronic heart disease. This is no longer the case, nor is it recommended to prevent cognitive decline and dementia. However, HGH and testosterone therapies do provide many of those benefits. That is why we highly recommend speaking with a hormone specialist that focuses on working with aging adults over 30 who want to keep their essential hormone levels in balance for optimum well-being.
Hormone therapy for menopause brings numerous benefits that can improve a woman’s quality of life.
Risks and Side Effects of Hormone Therapy
The older a woman is, the riskier it is to begin or stay on hormone replacement therapy. HRT use should be given in the lowest effective dosage for the shortest time. Hormone therapy for menopause treatment can last for up to ten years, if necessary. Some women experience hot flashes for well beyond the recommended five years of treatment. The age of sixty is considered a viable cutoff to end HRT unless symptoms persist beyond this point. Some women may continue receiving treatment up until sixty-five if symptoms remain persistent or impair quality of life.
The use of ET or EPT is contraindicated if the patient is at high risk for breast cancer . Mammograms are recommended starting at age 40 and are useful tools to monitor a woman’s risks while taking any form of estrogen hormone therapy. Females who have a family history of chronic heart disease should also discuss HRT with a qualified physician. Liver disease, prior stroke or blood clot, unexplained vaginal bleeding, transient ischemic attack, or endometrial (uterine) cancer may also eliminate the use of estrogen-based treatments. Because oral estrogens do pass through the liver, these could cause further risks. EPT that utilizes synthetic progestin rather than bioidentical progesterone can increase the risk of adverse events.
Hormone therapy for menopause should consist of the lowest effective dosage for the shortest time.
Measuring the Pros and Cons of Hormone Therapy for Menopause
It is vital for every woman to weigh the pros and cons of HRT for menopause with a hormone specialist. Even if one has a risk factor that precludes estrogen therapy, other options exist that may provide benefits without side effect concerns. The younger a woman is at the start of hormone therapy, the better.
The most important question to ask is, do the benefits outweigh the risks?
Hormone deficiency can increase the following risks:
- Trusted sourceWhat Is Dementia?Alzheimers AssociationGo to sourceDementia
- Osteoporosis
- Cardiovascular disease
- Type 2 diabetes
- Possibly an increase in weight gain
The use of hormone therapy for menopause treatment is extremely safe for most females. Those who have mitigating circumstances due to individual or family risk factors can often use other, safer options.
Using safe HRT for menopause can greatly impact one’s quality of life. For women who suffer from severe hot flashes, night sweats, and mood swings, just getting through each day can be difficult. Hormone therapy can significantly reverse that scenario.
It is essential to discuss with a doctor and weigh the pros against the cons of hormone replacement.
How to Select the Right Type of Hormone Therapy
Selecting the right treatment for one’s needs is of paramount importance. What is the best HRT for menopause? That is where the expertise of a knowledgeable hormone specialist is invaluable.
The HRT physician will first measure your blood levels of numerous hormones to determine where your deficiencies lie. The proper treatment will address those needs, along with taking into consideration your health status and symptoms. Customized HRT provides the best outcome with the least risk.
Oral estrogens can further lower testosterone levels and lead to a condition called “estrogen dominance.” When this occurs, weight gain and low libido are likely. Estrogen consumed orally also increases the risk of blood clots and stroke.
Low dose estrogens administered vaginally or via transdermal preparations are considerably safer to use. Remember, vaginal preparations treat only local symptoms and will do nothing for night sweats or hot flashes.
If the uterus is intact, then progesterone is necessary to use along with an estrogen treatment. The medical profession has long stated that women who do not have a uterus due to a hysterectomy do not require progesterone. However, progesterone as a hormone has numerous functions that are vital to a woman’s health. That is why a hormone specialist will verify progesterone levels before prescribing treatment options.
Stopping hormone therapy for menopause treatment is best when tapered off if using estrogen therapy. The abrupt end of treatment could cause a return of hot flashes and other unwanted symptoms.
For answers to any questions about the many types of hormone therapy available to treat menopause symptoms, please contact our clinic for a free consultation.
- Tomas Fait MD, PhD
- Bushra Imtiaz, MD, MPH, Marjo Tuppurainen, Toni Rikkonen, PhD, Miia Kivipelto, MD, PhD, Hilkka Soininen, MD, PhD, Heikki Kröger, MD, PhD, Anna-Maija Tolppanen, PhD
- Nancy F Woods, PhD, RN, FAAN, Wulf H Utian, MB.BCh., PhD., DSc
- Rogerio Lobo, M.D., Kathyrn Martin, M.D., Christine Burt Solorzano, M.D.
Menopause hormone therapy: latest developments and clinical practice
Postmenopausal hormone therapy and Alzheimer disease
Impact of hormone therapy on quality of life after menopause