Contents
- What Is Osteoporosis?
- Osteoporosis Causes
- Which Hormones Regulate Bone Growth?
- What is the Connection Between HGH Deficiency and Osteoporosis?
- Does HGH Increase Bone Density?
- The Effects of Growth Hormone on Cortical and Cancellous Bone
- Growth Hormone Reduces Risk of Osteoporosis Fractures
- Benefits of HGH for Strengthening Bones and Reducing the Risk of Osteoporosis
- What Does the Research Have to Say About HGH and Bone Health?
- Other Benefits of Growth Hormone Therapy
Multiple research studies have shown that HGH can be used to improve bone health and reduce the risk of osteoporosis and osteoporosis-related fractures.
As we get older, we struggle with numerous health issues, a major one being the increased risk of osteoporosis. The greatest risk to people with osteoporosis is bone fractures. Fractures are common in people with osteoporosis because it usually occurs around the same time that people start to experience balance, weakness, and other issues that can cause falls. Fractures are also harder to heal in older people, making osteoporosis fractures particularly dangerous.
A landmark study published in 2015 in the Endocrine Society’s Journal of Clinical Endocrinology & Metabolism found that for many years after it was given, HGH continued to reduce the risk of fractures and helped maintain bone density in postmenopausal women who had osteoporosis.
Since then, a recent literature review and meta-analysis indicated that growth hormone replacement therapy reduces the risk for fracture in all patients with osteoporosis, men, and women.
Studies have proven that HGH can strengthen bones and prevent fractures typical of osteoporosis.
What Is Osteoporosis?
Osteoporosis is a degenerative bone disease. Osteoporosis is more common in women, but it affects nearly 200 million people all around the world, both men and women. Osteoporosis is the cause for the weakening of bones that leads to fractures that are common among the elderly. Osteoporosis also makes these fractures difficult to heal, so osteoporosis fractures can be severely disabling to older people.
Osteoporosis Causes
Numerous health conditions and certain types of medical procedures can significantly influence the development of osteoporosis. The National Osteoporosis Foundation provides a comprehensive listing of health conditions and medications that could potentially contribute to osteoporosis. The box below features some of the most common causes separated into categories for easy viewing (This is not a complete list):
| Autoimmune Disorders | Lupus, Multiple Sclerosis, Rheumatoid Arthritis |
| Cancer | Breast Cancer, Prostate Cancer |
| Digestive and Gastrointestinal Disorders | Celiac Disease, Colitis, Crohn’s Disease |
| Endocrine and Hormonal Disorders | Cushing’s Syndrome, Diabetes, Hormone Deficiencies, Hyperthyroidism, Irregular Periods, Premature Menopause |
| Hematologic/Blood Disorders | Leukemia, Lymphoma, Multiple Myeloma, Sickle Cell Disease |
| Mental Illness | Depression, Eating Disorders |
| Neurological/Nervous System Disorders | Multiple Sclerosis, Parkinson’s Disease, Spinal Cord Injuries, Stroke |
| Other Conditions and Diseases | Chronic Kidney Disease, Chronic Obstructive Pulmonary Disease (COPD) including Emphysema, Female Athlete Triad (loss of menstrual periods, eating disorder, excessive exercise), HIV/AIDS, Liver Disease (Biliary Cirrhosis), Malnutrition, Organ Transplants, Poor Diet,Scoliosis |
| Medical Procedures | Gastrectomy, Gastrointestinal Bypass Procedures, Weight Loss Surgery |
| Medications | Antacids containing aluminum, Antiseizure – specific brands, Cancer chemotherapy drugs, Glucocorticoids (steroids) – cortisone, prednisone, Heparin Methotrexate, Thyroid hormones – excessive use |
Which Hormones Regulate Bone Growth?
Both human growth hormone (HGH) and testosterone play a vital role in bone health. Of the two, HGH is more important as it is instrumental to both bone and muscle growth. Since it is muscles that provide support for skeletal bones, muscle and bone are intricately related. Stronger muscles mean stronger bones and a lowered risk of osteoporosis-related fractures.
What is the Connection Between HGH Deficiency and Osteoporosis?
HGH has been scientifically proven to be able to prevent and treat osteoporosis.
HGH is produced by the pituitary gland. It is instrumental for bone and muscle growth and repair. Since HGH is known to influence and enhance the growth of every tissue in the body, it makes perfect sense that growth hormone therapy would be a beneficial treatment and prevention method for osteoporosis. Many published studies have proven that HGH therapy can reduce or prevent osteoporosis fractures in older people.
Postmenopausal women are most at risk of developing osteoporosis. HGH therapy has proven to be particularly useful in preventing fractures in this group of patients.
At the same time, as it is increasing your bone density, HGH also improves lean muscle mass. It is the body’s muscles that support and protect the bones from damage. Helping to build and strengthen muscle is another way that HGH works to prevent fractures in older men and women.
Does HGH Increase Bone Density?
As a child grows into an adult, it is HGH that is primarily responsible for the bone growth that results in longer bones, which makes us grow taller.
That process of bones growing longer and stronger is known as “bone remodeling.” It is the process of new bone formation by osteoblasts (cells that form new bone) and bone resorption by osteoclasts.
HGH directly and through IGF-I stimulates osteoblast proliferation and activity, promoting bone formation. It also stimulates osteoclast differentiation and activity, promoting bone resorption. The result is an increase in the overall rate of bone remodeling, with a net effect of bone accumulation and increased bone density.
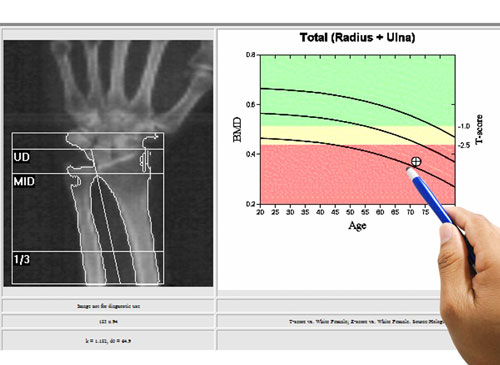
As HGH levels drop in elderly adults, it results in a reduced rate of bone remodeling and a gradual loss of bone mineral density.
In addition to helping to heal osteoporosis-related fractures, HGH can also help prevent such fractures by strengthening bone.
The Effects of Growth Hormone on Cortical and Cancellous Bone
There are two types of bone in the human body — cortical bone, also known as compact bone, and Trabecular bone, also known as cancellous or spongy bone. Cortical bone is much denser, with porosity ranging between 5% and 10%.
In studies, human growth hormone has been shown to have a positive effect on the strength, health, and density of both types of bone.
Growth Hormone Reduces Risk of Osteoporosis Fractures
HGH has been shown to help prevent osteoporosis fractures in a number of ways. First and foremost, HGH can improve bone density and make up for the bone loss typical of patients with osteoporosis. HGH also can help patients lose weight, which puts less pressure on bones. HGH therapy also helps to build muscle and ligaments, which support bones, improve balance, and strengthens the overall musculoskeletal system.
Benefits of HGH for Strengthening Bones and Reducing the Risk of Osteoporosis
HGH has been scientifically proven to be able to prevent and treat osteoporosis. Osteoporosis is referred to as a degenerative bone disease because it causes less bone mass to be produced in relation to the amount of old bone that is resorbed. The result of more bone being cells being lost than are replaced leads to weaker, less dense bones.
Research has proven that HGH, with its known ability to enhance cellular rejuvenation and tissue growth, can be a remarkable treatment and prevention method for osteoporosis.
If you are over 40 years of age, there has never been a more critical time than now to learn about HGH and osteoporosis. We know now conclusively that human growth hormone plays a crucial role in protecting bone density and decreasing the risk of fractures.
What Does the Research Have to Say About HGH and Bone Health?
Studies around the world are reporting the benefits of HGH for osteoporosis and bone health.
A recent study published in the Journal of Clinical Endocrinology & Metabolism proved that the HGH helps to reduce the risk of fractures and maintain the bone mass within healthy levels among postmenopausal women who have been diagnosed with osteoporosis. Furthermore, that study indicated the results of HGH treatment for osteoporosis were long-lasting, concluding, “A decade after the study began, the women who received the larger growth hormone dose still had higher bone mineral density levels than the participants who received the lower dose or the placebo.”
A 2018 study concluded, “Patients who received HGH had a significant decrease in fracture risk as compared to control.”
Earlier studies said that “Treatment of osteoporosis with HGH is found to be beneficial due to the increased bone metabolism and improved bone geometry which occurs with HGH.” Another study in that same year in 1998 concluded that “GH treatment for more than 18 months gives increased bone formation and bone mineralization of newly produced bone and a concomitant increase in bone mass as determined with DEXA. Thus, the action of GH on bone metabolism in GHD adults is 2-fold: it stimulates both bone resorption and bone formation.”
Another study in 2000 discovered that “HGH increases bone formation both via direct interaction with growth hormone receptors on osteoblasts and via locally produced IGF-I HGH deficiency results in decreased bone mass in both man and laboratory animals and treatment of growth hormone deficient patients with HGH for several months results in increased bone mass. HGH treatment also increases bone mass and the total mechanical strength of bones in rats with normal HGH secretion.”
Soon after, in 2002, a study on HGH and bone density concluded by saying, “In conclusion, this study showed that HGH treatment of men with idiopathic osteoporosis continuously, as well as intermittently, in combination with calcium and vitamin D3 for two years resulted in an increase in BMD (bone mineral density) in the lumbar spine and total body and an increase in total body BMC (bone mineral content), which was sustained, and possibly also increased further, for at least one year post-treatment.
Then again, in 2017, a “meta-analysis” (a study of studies) published in the journal Rheumatology Advisor concluded that “A recent literature review and meta-analysis indicates that growth hormone therapy can reduce the risk for fracture in patients with osteoporosis.”
Growth hormone therapy can help treat or lower the risk of osteoporosis fractures in older adults.
Other Benefits of Growth Hormone Therapy
Multiple studies have shown that HGH has the ability to improve bone mass and bone density, which helps to reverse the bone loss of osteoporosis. Improving bone health is just one of the many benefits of growth hormone therapy.
In addition to strengthening bones and reducing the risks of osteoporosis, growth hormone therapy:
- Improves fat metabolism and results in more lean muscle and less fat
- Increase energy and vitality
- Improves skin health, lessens the appearance of creepy skin, line, and wrinkles
- Improves sleep
- Increases cognitive functioning
- Improves heart health and lower the risk of cardiovascular disease
- Boosts your immune system
- Improves mood
- Increases libido and improves sexual function
FAQ
- Hayden Atkinson, PhD, Dr. Rebecca Moyer, Daniel Yacoub, PhD, Dexter Coughlin, Trevor Birmingham, PhD
- Maya Barake, MD, MSc, Anne Klibanski, MD, Nicholas A Tritos, MD, DSc
- Emily Krantz, MD, Penelope Trimpou, MD, PhD, Kerstin Landin-Wilhelmsen
- Kerstin Landin-Wilhelmsen, Anders Nilsson, Ingvar Bosaeus, Bengt-Ake Bengtsson
- Peter Gillberg, Hans Mallmin, Marianne Petrén-Mallmin, Sverker Ljunghall, Anna G. Nilsson
- Vittorio Locatelli and Vittorio E. Bianchi
Effects of Recombinant Human Growth Hormone for Osteoporosis: Systematic Review and Meta-Analysis
Effects of Recombinant Human Growth Hormone Therapy on Bone Mineral Density in Adults With Growth Hormone Deficiency: A Meta-Analysis
Effect of Growth Hormone Treatment on Fractures and Quality of Life in Postmenopausal Osteoporosis: A 10-Year Follow-Up Study
Growth hormone increases bone mineral content in postmenopausal osteoporosis: a randomized placebo-controlled trial
Two Years of Treatment with Recombinant Human Growth Hormone Increases Bone Mineral Density in Men with Idiopathic Osteoporosis
Effect of GH/IGF-1 on Bone Metabolism and Osteoporsosis