Testosterone Therapy After Prostate Cancer
Contents
The use of testosterone after prostate cancer has long been a controversial subject. For years, many in the medical field have argued that the incidence of prostate cancer increases with age, at the same time that testosterone levels decline. That theory alone shows the connection between testosterone and prostate health. If higher levels of testosterone were the cause for prostate cancer, then men would be more likely to develop it at a younger rather than an older age.
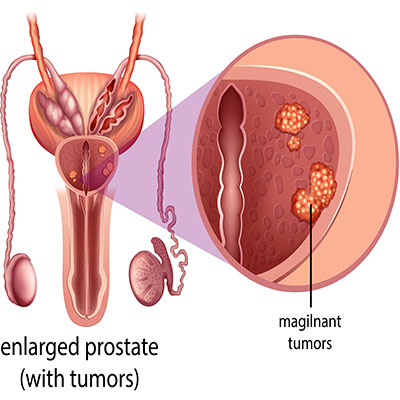
In truth, testosterone may be protective for prostate health, keeping Trusted sourceDihydrotestosteroneHormone Health NetworkGo to sourcedihydrotestosterone (DHT) levels in balance. DHT is a result of testosterone conversion by the enzyme 5-alpha reductase. In older men, increased DHT conversion causes an imbalance as testosterone levels decline in relation to DHT. Dihydrotestosterone plays a role in prostate enlargement as well as hair loss.
Once thought to be contraindicated, testosterone therapy after prostate cancer has many benefits for men.
Prostate Cancer Overview
Prostate cancer rarely occurs before age 50, although it is a possibility. PC is a slow growing disease, often without symptoms until it reaches an advanced stage.
It is important to study the use of testosterone replacement after prostate cancer because men with PC typically have low testosterone levels. Low T adversely impacts the quality of life (QoL).
Depression is common in both Low T and PC, often negatively influencing a man’s day to day activities. TRT can help improve emotional and physical well-being, enhancing overall QoL.
Here are some facts about prostate cancer:
Causes and Symptoms
The cause of prostate cancer is unknown. Most men will experience enlargement of the prostate gland as they age.
Prostate enlargement can impact urinary functions, often causing the following symptoms:
- Weak urinary stream
- Urinary urgency
- Frequent waking at night
- Bone pain – in advanced stages
Risk factors
Certain factors contribute to an increased Trusted sourceProstate Cancer: Risk Factors and PreventionDoctor Approved Patient Information from ASCOGo to sourcerisk of developing prostate cancer , including:
- Diet – this is considered one of the leading risk factors. Men who consume large quantities of dairy and red meat, but very little vegetables have an increased risk of PC.
- Race – aggressive prostate cancer is more common in men of African-American descent, but all men are at risk.
- Aging – the most common age of diagnosis is for men in their 60s and 70s.
- Family history – risk increases for men who have a relative also diagnosed with PC. When due to familial relationships, prostate cancer may develop at an earlier age. The following genes may be related to an increased PC risk: BRCA1, BRCA2, and HOXB13.
- Lifestyle – obesity, alcohol abuse, toxic chemical exposure, lack of exercise, and a sedentary lifestyle increase PC risk.
Many males have no idea that they have prostate cancer. Except in very rare, aggressive forms of the disease, it is not likely for one to die from PC.
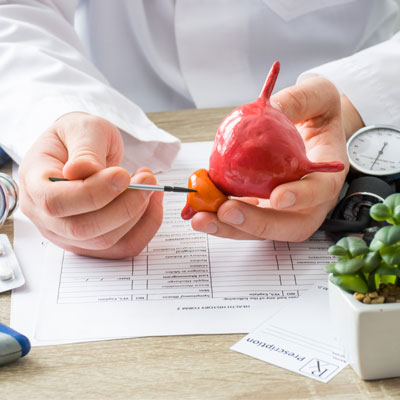
Treatment for prostate cancer may include:
- Surgical removal of the prostate gland – radical prostatectomy removes the entire prostate, some surrounding tissue, and seminal vesicles.
- Radiation therapy – often used for a first treatment when PC is low grade and confined to the prostate gland, as well as those that have spread into nearby tissue. Also used when not all PC is removed during surgery (or in cases of recurrence), as well as to help relieve symptoms in advanced stages.
- Watchful waiting – less intense observation through fewer tests and focusing on any changes in symptoms.
- Active surveillance – close monitoring through PSA blood tests and digital rectal exams every six months and possible prostate biopsies yearly.
- Cryotherapy (cryosurgery or cryoablation) – may be used to freeze and destroy prostate tissue.
- Hormone therapy – also called androgen deprivation or suppression therapy, ADT reduces testosterone levels to impede their influence on the prostate. Recent studies have shown that higher testosterone levels do not necessarily influence prostate cancer growth and lowering testosterone levels may cause more harm by weakening bones, reducing metabolic functions, and decreasing quality of life.
- Chemotherapy – A may be used if hormone therapy does not work and cancer has spread outside the prostate gland.
- Immunotherapy – A man’s white blood cells are removed and treated with a protein that will help the cells to recognize and target diseased prostate cancer cells. The treatment is given through an intravenous (IV) infusion. Although not a cure, the treatment may help men with advanced PC live several months longer.
There is also the use of testosterone therapy after prostate cancer to help improve QoL.
Prostate cancer risk increases as men age and their testosterone levels decline.
Does Testosterone Increase the Risk of Prostate Cancer Recurrence?
The concern for prostate cancer recurrence following successful treatment is a valid one. No man wants to go through prostate cancer a second time, especially if he has been cured. In the past, it was thought that since testosterone and DHT exist in the prostate, increasing their levels would cause prostate cancer to grow. That is not the case.
A new saturation model has emerged that shows that while increasing testosterone levels with testosterone therapy after prostate cancer boosts the amount of the hormone in the bloodstream, it does not raise the level in the prostate. Once prostate cells reach their saturation point with testosterone, there is no further increase in testosterone concentration in the prostate.
For that reason, the use of supplemental testosterone after prostate cancer has not been shown to increase the risk of recurrence.
The prostate gland has a saturation point for testosterone and increasing blood testosterone levels will not increase PC risk.
Testosterone and Prostate Cancer Research
At the 2018 American Urological Association meeting held in San Francisco, doctors reported that administering testosterone therapy after prostate cancer treatment does not increase recurrence or progression rate.
According to one of the leading experts in the field, Trusted sourceDr. Abraham MorgentalerA4M MMIGo to sourceDr. Abraham Morgentaler , MD, the Director of Men’s Health Boston and Associate Clinical Professor of Urology at Harvard Medical School in Boston, recurrence rates for men treated with testosterone following surgery or radiation for PC were low. The same was true for men undergoing active surveillance and no testosterone.
Another 2018 report, “Shifting the Paradigm of Testosterone Replacement Therapy in Prostate Cancer” discussed the Saturation Mmodel. When we look at low testosterone and prostate cancer, we find that it affects roughly 30 percent of men between the ages of 40 and 79. The percentage increases with age. An analysis of 18 prospective trials of 3,866 men with PC compared to 6,439 controls showed no association between prostate cancer and prediagnostic testosterone levels.
In Trusted sourceTestosterone treatment is not associated with increased risk of prostate cancerGo to sourceanother study from 2017 of 999 men, 75% underwent TRT. The proportion of positive biopsies was identical in men who received testosterone compared to those who did not – 37.5% and 37.0% respectively.
Continuing research has shown no increase in prostate cancer risk from testosterone therapy.
Prostate Cancer Prevention
Prevention is the number one word to consider if you are a male over the age of 40. Your testosterone levels are already declining, so you need to be proactive to maintain healthy testosterone production while avoiding actions that could increase PC risk. We know that there is no direct connection between testosterone and prostate cancer as far as treatment goes. What we do suspect is that maintaining healthy testosterone levels will help reduce prostate growth.
To protect your testosterone production, as well as for how to increase testosterone after prostate cancer, focus on the following:
- Getting between 7 and 9 hours of quality sleep each night to maintain healthy hormone secretion
- Reducing stress to lower cortisol levels which can inhibit testosterone
- Increasing the intake of heart-healthy fats, fruits, and vegetables
- Avoiding sugar and red meat
- Exercising
- Losing weight
To reduce the risk of prostate cancer, consider these steps:
- Increase consumption of vegetables and fruit
- Reduce dairy consumption
- Limit red meat intake to no more than 2 times a week
- Opt for low-fat when you do choose dairy
- Exercise
- Lose weight if you are overweight
If you have Low T that is preventing you from getting adequate sleep and exercise due to fatigue or joint pains, then testosterone therapy after prostate cancer can help reduce further risks by reversing those concerns.
You can take proactive steps to improve testosterone levels and reduce prostate cancer risk.
Does Taking Testosterone Decrease the Risk of Prostate Cancer?
The final word on prostate cancer and testosterone is this – TRT has not been shown to increase the risk of developing PC, and it may decrease the risk through its protective impact on the prostate. Remember, when DHT levels rise, and testosterone levels decline, the body is no longer in hormonal balance. A hormone specialist can provide the appropriate treatment to restore balanced hormone levels.
For additional information about receiving testosterone therapy after prostate cancer, please contact HGH Doctor hormone clinic for a confidential consultation. There is no charge for this call, so get the information you need for a healthy tomorrow.
- Ranjith Ramasamy, MD., Erik S. Fisher, Peter N. Schlegel, MD., F.A.C.S.
- Alexander W. Pastuszak, MD., PhD., Katherine M. Rodriguez, MD., Taylor M. Nguyen, MD., Mohit Khera, MD., MBA., MPH., Prof.
- Peter Celec, Assoc. Prof., MD, Dipl. Ing., MSc., PhD., MPH., Daniela Ostatníkovám Prof., PhD., Július Hodosy, Assoc. prof., MD., MSc., PhD., MPH.
- Alexander W Pastuszak, MD., PhD., Amy M Pearlman, MD., Win Shun Lai, MD., Guilherme Godoy, MD., Kumaran Sathyamoorthy, MD., Joceline S Liu, MD., Brian J Miles, MD., Larry I Lipshultz, MD., Mohit Khera, MD., MBA., MPH.
- Taylor M. Nguyen, MD., Alexander W. Pastuszak, MD., PhD.
- Thomas E Ahlering, MD., Linda My Huynh, Maxwell Towe, Kaelyn See, Joshua Tran, Kathryn Osann, Farouk M El Khatib, Faysal A Yafi
Testosterone replacement and prostate cancer
Testosterone therapy and prostate cancer
Testosterone therapy does not increase the risks of prostate cancer recurrence or death after definitive treatment for localized disease
Testosterone replacement therapy in patients with prostate cancer after radical prostatectomy
Testosterone Therapy Among Prostate Cancer Survivors
On the Testosterone replacement therapy reduces biochemical recurrence after radical prostatectomy