Testosterone Replacement Therapy after Radical Prostatectomy
Contents
- Other Options to a Radical Prostatectomy for the Treatment of Prostate Cancer
- What Is a Radical Prostatectomy?
- Can Testosterone Therapy Help Avoid a Radical Prostatectomy
- Can it do the same for men with prostate cancer?
- What Does Testosterone Therapy do After a Radical Prostatectomy?
- Benefits for Erectile Function from Testosterone Therapy after a Radical Prostatectomy
If a man undergoes a radical prostatectomy, he will have a long recovery road ahead of him. Due to the challenges of surgery, it is common for depression and mood changes to occur. Because testosterone levels decline with age, and testosterone influences brain functions, this adds a second contributing factor for depression. Therefore the use of testosterone therapy after radical prostatectomy can benefit and improve overall mood and quality of life.
Current research backs up the safe use of testosterone therapy following radical prostatectomy. Trusted sourceTestosterone replacement therapy in patients with prostate cancer after radical prostatectomyNational Library of MedicineGo to sourceStudies following TRT after radical prostatectomy have shown a rise in PSA levels, but no increased risk of prostate cancer recurrence.
Testosterone replacement therapy following radical prostatectomy is safe and can help reduce feelings of depression.
Other Options to a Radical Prostatectomy for the Treatment of Prostate Cancer
Trusted sourceRadical prostatectomyJohns Hopkins Medicine Go to sourceRadical prostatectomy is not the only treatment for prostate cancer. We already know that the use of testosterone replacement therapy after radical prostatectomy is safe and beneficial for many males, but what about other options?
There are options for treating prostate cancer (PC) that include:
- Active surveillance or watchful waiting – monitoring the situation
- Radical prostatectomy – surgery to remove the prostate gland
- Radiation – often used first in low-grade PC or following surgery if cancer has spread outside the prostate gland
- Androgen deprivation therapy – using hormones to suppress the growth of prostate cancer cells that multiply via testosterone signaling
- Cryotherapy – freezes and destroys prostate tissue
- Chemotherapy – when hormone therapy does not work on PC that has spread
In addition to utilizing testosterone treatment after radical prostatectomy, TRT can also be beneficial in many of these other options.
Numerous options exist for the treatment of prostate cancer.
What Is a Radical Prostatectomy?
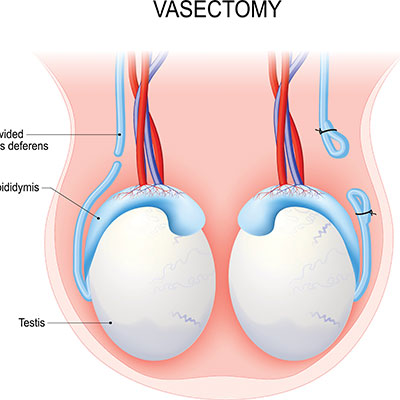
A radical prostatectomy is a surgical procedure resulting in the removal of the entire prostate gland. It is a common procedure for men whose prostate cancer remains localized in the prostate. Before we talk further about using testosterone after radical prostatectomy, let us explore more about what this surgery accomplishes. When you removed the diseased prostate, you take the tumor out of the body – providing it has not spread beyond the prostate.
There are two primary methods of removing the prostate gland:
- Open radical prostatectomy – the prostate is surgically removed through an incision in the lower abdomen
- Laparoscopic radical prostatectomy – several small incisions in the abdomen allow for insertion of a laparoscope, which is a long and slender device with a camera. Other instruments can be inserted alongside the laparoscope to perform the surgical procedures.
Studies suggest that men experience a shorter recovery time with laparoscopic surgery. In cases of recurring or advanced prostate cancer that has spread beyond the prostate gland, removal of the lymph nodes or radiation is possible.
Recovery time is significant following surgery, requiring restricted activity for a few months allowing the abdomen time to heal. Incontinence or urinary leakage is another possibility which could take up to a year to improve.
Radiation therapy helps lower the recurrence rate in men with T3-T4 disease or lymph node involvement. T3-T4 refers to PC with a positive margin – meaning the disease has spread outside the prostate capsule (connective tissue layer around the prostate). Some doctors prefer to wait and use radiation only if a detectable rise in PSA levels occurs.
How can PSA levels rise following radical prostatectomy? If there is no prostate gland, it would seem impossible for the body to produce prostate-specific antigen. However, it is possible for some prostate cancer cells to spread outside the treatment area, and begin to multiply (metastasize). When that occurs, there is potential for PSA levels detectable by lab tests. PSA monitoring following radical prostatectomy is a primary indicator of whether all prostate cancer cells were destroyed.
For some men with lymph node involvement, hormone therapy in the form of Trusted sourceAndrogen Deprivation Therapy in the Treatment of Advanced Prostate CancerNCBIGo to sourceandrogen deprivation therapy (ADT) is useful, especially in metastatic prostate cancer. By blocking testosterone production or from testosterone acting on PC cells, ADT can help prolong life span. However, it can lead to a significant decline in testosterone levels that can cause decreased bone density, erectile dysfunction, weight gain, depression, and many other Low T symptoms.
A radical prostatectomy is a surgical procedure that removes the prostate gland.
Can Testosterone Therapy Help Avoid a Radical Prostatectomy
The avoidance of any surgery is always a good thing – when possible. Anytime you cut into the body; there are inherent risks. In this section, we discuss the possibility of avoiding a radical prostatectomy. Testosterone therapy has been shown to help improve male lower urinary tract symptoms in some patients with benign prostatic hyperplasia – prostate enlargement.
Can it do the same for men with prostate cancer?
We already know that androgen deprivation therapy which reduces testosterone levels can help decrease the prostate size and improve urinary functions for some men. If that is true, then how can the reverse – increasing testosterone levels – do the same thing?
Preliminary research has begun to show that the use of finasteride (a drug typically used to treat benign prostatic hyperplasia and male pattern baldness) may help prevent the occurrence of certain types of prostate cancer. While testosterone therapy does not directly prevent or avoid a radical prostatectomy, finasteride may help reduce the development of prostate cancer indirectly.
Remember, even with testosterone levels declining with age, prostate growth continues. Again, we point out the saturation model that shows that the prostate is fairly insensitive to changes in testosterone concentration at normal or mildly low levels. However, in extreme hypogonadism, the prostate is sensitive to changing androgen levels – hence the use of ADT.
Several studies have shown that men under active surveillance monitoring for low-risk prostate cancer who received TRT did not have an increased risk of prostate cancer advancement.
In addition to the use of testosterone replacement therapy after radical prostatectomy, some hypogonadal men may also benefit from receiving TRT before undergoing surgery.
Although testosterone therapy does not “cure” prostate cancer, it may be safe for a man to use before undergoing radical prostatectomy, and may help with some of the PC symptoms.
What Does Testosterone Therapy do After a Radical Prostatectomy?
Following radical prostatectomy, a man will remain in the hospital for one to two days and then go home with a catheter for one to two weeks to help drain urine from the body. Over the next few months, urinary leakage or incontinence is common. We previously mentioned the likelihood of depression, which is one reason for using testosterone replacement after radical prostatectomy. As testosterone levels increase, signals to the androgen receptors in the brain increase, promoting a sense of well-being.
Additionally, because low testosterone often causes a decline in bone and muscle mass, a man is at an increased risk of developing osteoporosis. The body becomes structurally weak. Weight gain is likely. In addition to contributing to feelings of depression, these changes also impact self-image.
Low testosterone levels also interfere with sleep, leading to a surge in cortisol (stress hormone) secretion. Cortisol inhibits sleep, leading to a further decline in testosterone and growth hormone production. Lack of sleep causes fatigue, impaired cognitive functions, and overeating to compensate for low energy levels.
Testosterone replacement therapy after radical prostatectomy can help reverse a some of those symptoms. Because TRT also exerts a positive influence on cholesterol and blood pressure levels, it may aid the heart in increasing exercise capacity which can help your surgical recovery.
Testosterone replacement therapy helps improve energy, sleep, mood, and bone and muscle strength.
Benefits for Erectile Function from Testosterone Therapy after a Radical Prostatectomy
Erectile dysfunction is a concern for many males, especially following radical prostatectomy. Testosterone levels that are low can cause a decline in sexual desire and arousal. The most common side effect of radical prostatectomy is erectile dysfunction.
Why does surgical prostate removal increase the risk of ED?
A network of blood vessels and nerves that run along the sides of the prostate are crucial for normal erectile functions. However, because of their proximity to the prostate gland, it is natural for them to undergo some form of disturbance during the surgery. It is often possible to spare the nerves when the tumor remains confined to the prostate gland. If cancer has spread beyond the prostate, it might impact some of the nerves. That can cause a change in erectile functions.
Because the penis also requires oxygen to help with engorgement, you need an adequate blood supply to reach the organ. Testosterone is a stimulator of red blood cell production in bone marrow. The use of testosterone replacement therapy after radical prostatectomy can help improve blood circulation and therefore increase the supply of oxygen-rich blood to the penis.
Finally, because testosterone also works on the brain, where androgen receptors help stimulate sexual desire, you have benefits on all fronts. Testosterone not only increases libido, but it helps improve sexual functions and pleasure.
To learn more about the use of testosterone replacement therapy following treatment for prostate cancer, please contact HGH Doctor. Our hormone specialists are available for free, confidential consultations by phone, so contact us today.
Testosterone replacement therapy helps to improve sexual desire, arousal, and erectile functions following radical prostatectomy.
- Alexander W Pastuszak, md, pHd, Dr. Amy M. Pearlman, MD, Dr. Win Shun Lai, MD, Dr. Guilherme Godoy, MD, Dr. Kumaran, Sathyamoorthy, MD, Joceline S Liu, MD, Dr. Brian J. Miles, MD, Dr. Larry Lipshultz, MD, Mohit Khera, MD, MBA, MPH
- Joel M. Kaufman, MD, Dr. R. James Graydon, MD
- Dr. Piyush K. Agarwal, MD, Michael G Oefelein, MA, FACS
- Fernanda G. Herrera and Dominik R. Berthold
- Thomas E Ahlering, Linda My Huynh, Maxwell Towe, Kaelyn See, Joshua Tran, Kathryn Osann, Farouk M, El Khatib, Faysal A Yafi
- Gerald Chodak, MD
Testosterone replacement therapy in patients with prostate cancer after radical prostatectomy
Androgen replacement after curative radical prostatectomy for prostate cancer in hypogonadal men
Testosterone replacement therapy after primary treatment for prostate cancer
Radiation Therapy after Radical Prostatectomy: Implications for Clinicians
Testosterone replacement therapy reduces biochemical recurrence after radical prostatectomy
AUA 2019: More Evidence That Testosterone May Be Safe After Treatment for Prostate Cancer