Contents
- What Is Parathyroid Hormone?
- What is parathyroid hormone activity, and how does it accomplish its functions?
- What does parathyroid hormone do for calcium’s effects on the nervous system?
- What Controls Parathyroid Hormone?
- What Happens If You Have Low Parathyroid Hormone Levels?
- Can You Have Too Much Parathyroid Hormone?
- How Do You Check Parathyroid Hormone Levels?
- What Can You Do About Parathyroid Hormone Imbalance?
You often hear about the thyroid gland and thyroid hormones, but not as much about parathyroid hormone. However, what you do not know about parathyroid can be detrimental to your health.
Maintaining proper parathyroid gland function is crucial to your well-being. Your bones and kidneys rely on an adequate supply of parathyroid hormone, also called parathormone, parathyrin, or PTH for proper functioning.
The regulation of serum calcium levels, bone density, and the avoidance of kidney stones all rely on the proper function of parathyroid gland hormones.
In this review, we will cover the following topics:
- The function of parathyroid hormone
- How the parathyroid glands produce and regulate hormone output
- What happens when parathyroid hormone levels are too low
- The impact of too much parathyroid hormone
- How to test parathyroid hormone levels
- How to balance parathyroid hormone
Parathyroid hormone is essential for regulating calcium levels in the blood and protecting bone density.
What Is Parathyroid Hormone?
Do not confuse parathyroid hormone with thyroid hormones. Although they sound similar and come from nearby glands, these hormones are quite different. Whereas one of the primary functions of thyroid hormones is to regulate metabolism, parathyroid hormone has no metabolic activity. Instead, its primary function is the regulation of calcium levels in the blood; something thyroid hormone does not effect.
What is parathyroid hormone activity, and how does it accomplish its functions?
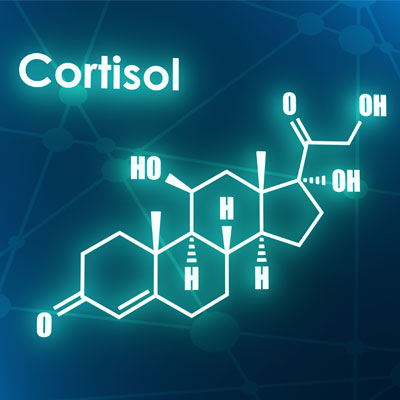
Parathyroid hormone is a polypeptide hormone containing 84 amino acids. PTH exerts its actions on the bones, intestines, and kidneys in the following ways:
- Bones: Calcium is stored in the bones. Parathyroid hormone triggers the release of calcium from bone deposits into the bloodstream. The action of the hormone helps control the amount of calcium in the bones – impacting their density and strength. Parathyroid hormone does this by stimulating the osteoclasts (bone-destroying cells) to reabsorb old bone mineral to release the stored calcium into the blood. In return, this allows for the completion of the bone remodeling process where old bone cells are absorbed, and new ones (osteoblasts) are created to fill in the empty spaces.
- Intestines: Here, parathyroid hormone helps improve vitamin D metabolism, which allows for more absorption of the calcium in food. PTH stimulates the production of the active form of vitamin D so that it can increase calcium-binding protein synthesis in intestinal epithelial cells that improve dietary calcium absorption into the blood.
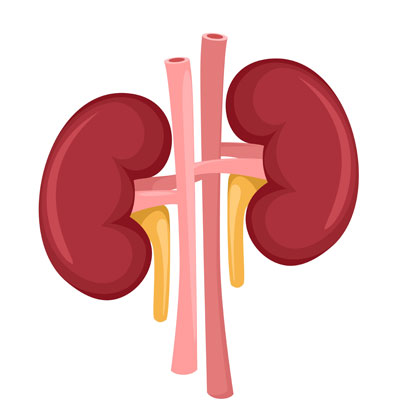
- Kidneys: The function of parathyroid hormone in the kidneys is to prevent the release of calcium in urine while increasing vitamin D production. PTH also stimulates the loss of phosphate ions in the urine.
What does parathyroid hormone do for calcium’s effects on the nervous system?
While this function of parathyroid hormone is discussed less frequently than that of its effects and influence on the bones, kidneys, and intestines, it is just as important. Calcium allows for normal electrical current conduction along the nerves so that they can communicate freely with one another. Calcium fluxes in and out of nerve cells, allowing them to pass their messages along. The brain requires calcium for proper functions. In addition, calcium is essential for muscle contraction.
We often do not give calcium and PTH enough credit for the work they do. It is easy to equate calcium only with the bones because that is what protects them and gives them their structural integrity. However, the real truth may be the other way around. The bones function as the brain’s storage house for the calcium that organ needs for proper functioning. When there is not enough calcium in the bloodstream, the brain may suffer.
Parathyroid hormone acts on the bones, kidneys, and intestines, to increase blood calcium levels.
What Controls Parathyroid Hormone?
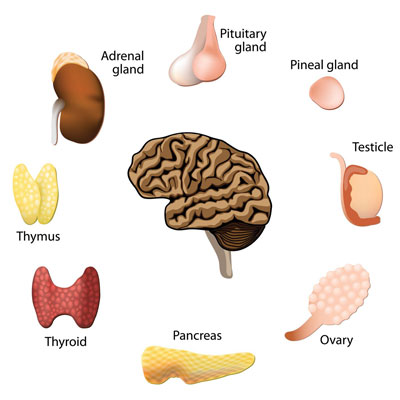
The parathyroid gland is the body’s producer of parathyroid hormone. Actually, there are four parathyroid glands, and they are located in the neck right behind the thyroid gland. The glands are about the size of a grain of rice. As with many other glands, the parathyroid glands receive specific signals telling them when to secrete parathyroid hormone into the bloodstream. In this case, it is blood calcium levels that prompt the hormone release.
The parathyroid glands contain calcium-sensing receptors that measure PTH levels in the bloodstream. You can also find these calcium sensors in bone marrow, the gastrointestinal mucosa, and the kidneys.
When the parathyroid glands’ calcium-sensing receptors sense low levels of calcium in the blood, additional parathyroid hormone is released to force the removal of calcium from the bones. If there are adequate or high levels of calcium in the blood, the glands stop secreting the hormone until the levels decrease.
The calcium range in the bloodstream varies only slightly. The feedback mechanism of the parathyroid glands sensing calcium levels and releasing parathyroid hormone is continuous, turning on and off dozens of times each day to maintain proper balance.
If a parathyroid gland loses its ability to regulate this balance, it can cause calcium levels to bounce around between high and low. A parathyroid tumor can cause this action called hyperparathyroidism.
The parathyroid glands measure the level of calcium in the blood to determine when to produce parathyroid hormone.
What Happens If You Have Low Parathyroid Hormone Levels?
Low parathyroid hormone, called Trusted sourceHypoparathyroidismNational Organization for Rare DisordersGo to sourcehypoparathyroidism , rarely occurs. When it does, it can lead to hypocalcemia or low blood calcium levels. Hypoparathyroidism most often occurs due to damage or removal of the parathyroid glands.
Low levels of parathyroid hormone can result in a tingling sensation in the fingers or around the mouth. Hand muscle cramps are also possible. The most severe symptoms (extremely rare) include severe muscle cramping of the entire body and convulsions. Sudden declines in calcium levels (often following a parathyroid surgery) can cause a foggy-headed or confused type of feeling. That is why calcium pills are essential when the body does not have enough calcium.
The brain cannot function properly as the nerve responses will not occur as they should. A person may feel as though their brain is not working right.
Low parathyroid hormone levels is rare and is most likely caused by damage or removal of the parathyroid glands.
Can You Have Too Much Parathyroid Hormone?
If abnormal parathyroid hormone function from the glands causes too much calcium in the blood, it is called hypercalcemia and referred to as primary hyperparathyroidism. Primary hyperparathyroidism is most often caused by an adenoma (parathyroid tumor) which results in too much PTH entering the bloodstream. Kidney stones and bone decalcification are common manifestations of this condition. There is sometimes an increased prevalence of insulin resistance and metabolism issues that can result in weight gain. That is the connection between parathyroid disease and weight gain. Radiation treatment to the neck, the drug lithium, and menopause increase the risk of this condition.
Secondary hyperparathyroidism is caused by conditions such as vitamin D deficiency or kidney disease that can result in low serum calcium levels. When the kidneys cannot reabsorb calcium, blood calcium levels decline, resulting in a continual output of PTH. Chronic kidney failure is the most common cause of secondary hyperparathyroidism. Vitamin D deficiency resulting from an inadequate diet or not getting enough sunlight can also lead to bone decalcification and fractures.
Tertiary hyperparathyroidism is even rarer and occurs due to all four parathyroid glands being overactive. It often follows an extended period of secondary hyperparathyroidism. Surgical removal of the parathyroid gland(s) is often required.
In mild cases of too much parathyroid hormone, there are rarely any symptoms. However, consistently and extremely elevated blood calcium levels can cause the following to occur:
- Complaints of illness with no apparent cause
- Constipation
- Depression
- Digestive upset
- Excessive thirst
- Forgetfulness
- Frequent urination
- Irritability
- Joint pain
- Lethargy
- Loss of appetite
- Nausea
- Poor sleep
- Weakness
- Weight gain
Another potentially dangerous aspect of having too much parathyroid hormone is that the bones continue releasing calcium into the bloodstream. By doing so, they are depleting the calcium stores in the bones that preserve bone density. When bone turnover and remodeling cannot keep up with the loss of calcium, the bones begin to weaken. That increases the risk of developing osteopenia and osteoporosis. If this condition continues untreated, the porous holes in the bones continue to grow, causing the bones to become brittle and prone to fractures.
Because calcium also helps muscles to contract, too much parathyroid hormone can result in muscular problems. Elevated calcium levels can cause problems with the liver, kidneys, and arteries, increasing the risk of strokes, kidney stones, and cardiac rhythm problems. Breast cancer risk may also increase.
Too much parathyroid hormone can lead to osteoporosis and cause numerous symptoms.
How Do You Check Parathyroid Hormone Levels?
The doctor will measure blood calcium levels, often as part of a routine blood test. Many people who have elevated calcium levels, and subsequently, too much parathyroid hormone often do not know it because there are rarely any symptoms. The same applies to having low calcium levels. That is why getting regular comprehensive blood testing each year is recommended.
Adults with normal calcium levels will have relatively zero variability in their calcium parathyroid test results. Calcium levels range 9 to 10.1 mg/dL.
If calcium levels drop below 9 or increase above 10.2, it is likely that you will not feel “well.” All adults over age 30 should have calcium levels no higher than 10.1. The mid 9 range is ideal. If an adult over 40 years of age has persistently high calcium levels above 10.1, it likely signals a parathyroid tumor. These tumors are benign – the only problem is that they cause too much parathyroid hormone to enter the bloodstream.
Routine blood analysis typically measures calcium levels.
What Can You Do About Parathyroid Hormone Imbalance?
If you have hypocalcemia, the doctor will likely treat the condition with oral vitamin D and calcium supplements. Calcium infusions may be beneficial for some people, especially if the parathyroid glands have been removed.
If too much parathyroid hormone causes elevated calcium levels due to a faulty gland or multiple parathyroid gland problems, the doctor may remove the affected gland(s) in a surgical procedure called a parathyroidectomy. Surgery is the most common treatment for primary hyperparathyroidism.
Following surgery for parathyroid gland removal, many people do lose weight. Also, treating hyperparathyroidism can also help with weight loss.
Parathyroid hormone treatment can help stimulate increased bone mass and strength with once daily injections. PHT therapy is effective for the treatment of osteoporosis in some people.
- Masafumi Fukagawa, Shohei Nakanishi, Hideki Fujii, MD, PhD, FASN, Yasuhiro Hamada, Takaya Abe
- Rajeenkanna Chilakapati, PhD, Chanchal Thomas, PhD student, Dr Krishna Kanth Pulicherla
- Andrew Mark Hinson, MD, Brendan C. Stack, MD, FACS, FACE
- Maqsood Khan, Alvin Jose, Sandeep Sharma
- Written by Amber Erickson Medically reviewed by Marina Basina, M.D.
- Benjamin Daniel Liess, MD; Chief Editor: Eric B Staros, MD
Regulation of parathyroid function in chronic kidney disease (CKD)
Prospects of Parathyroid Hormone in Therapeutic Intervention
Parathyroid Physiology and Molecular Biology
Physiology, Parathyroid Hormone
Parathyroid Hormone (PTH) Test