Contents
 The use of hormone therapy for endometriosis is the primary method of treating this condition that affects women. Some girls may develop endometriosis at a young age, even as early as a few years after starting their menstrual cycle.
The use of hormone therapy for endometriosis is the primary method of treating this condition that affects women. Some girls may develop endometriosis at a young age, even as early as a few years after starting their menstrual cycle.
Endometriosis tends to run in families, so if your mother had it, and you develop symptoms, you may want to see a doctor as soon as possible. The earlier you begin treatment, the better. Hormone therapy helps to reduce hormone spikes that occur during the menstrual cycle and reduce the symptoms of endometriosis.
Ignoring endometriosis can make it difficult to become pregnant, which is one reasonwhy treatment is beneficial. Trusted sourceHormone Treatments for endometriosisEndometriosisGo to sourceHormone therapy for endometriosis benefits a female by helping to prevent scarring and damage that canoccur because of natural hormone spikes during the menstrual cycle. These spikes are natural and harmless without endometriosis, but when endometriosis is present, long-term damage can occur. Since hormone treatment is usually a contraceptive, it will alsos prevent ovulation by stopping your periods. Your body will not be increasing the uterine lining to prepare for pregnancy. More about that in the next section.
Hormone therapy for endometriosis may not be an option in the following situations:
- If you smoke
- History of blood clots or stroke
- High blood pressure
- Severe active liver disease
- Heart disease
- Severe migraines
To diagnose endometriosis, the doctor will ask you about your symptoms and conduct a pelvic examination to feel for abnormalities in your pelvis. In addition, he or she may perform the following tests to determine if you have endometriosis, and, if so, how severe the condition is at this time:
- Ultrasound – this test is often done in the gynecologist’s office. It uses a high-frequency sound wave to create an image of the inside of the abdomen. The doctor may request an external ultrasound where the transducer device is pressed against the abdomen. The other option is an internal ultrasound where the device is inserted into the vagina. Ultrasound shows if there are cysts present but does not necessarily diagnose endometriosis.
- Magnetic resonance imaging (MRI) – using magnetic and radio waves, the doctor will see a detailed image of the tissues and organs in the abdomen. MRIs are useful before surgery to show the doctor where endometrial lesions are present.
- Laparoscopy – this is a surgical option that allows the doctor to see inside your abdomen while you are under general anesthesia. A tiny incision near the navel provides enough room for the slender laparoscope to see if there is endometrial tissue outside the uterus. The surgeon may remove a small sample of tissue to biopsy for additional testing. Many times, the doctor may also treat endometriosis during the laparoscopy, removing the endometrial tissue.
Hormone therapy is first-line treatment for endometriosis.
What Is Endometriosis?
When a woman has Trusted sourceEndometriosisU.S Department of Health & Human ServicesGo to sourceendometriosis , the inside lining of the uterus begins to grow outside the endometrium. It can affect the tissues lining the pelvis as well as the fallopian tubes and ovaries. Endometrial tissue is cyclical. It changes depending on the timing of the menstrual cycle.
Normal endometrial tissue sheds each month unless a woman is pregnant. When the tissue grows outside the uterus, it still undergoes the same thickening and shedding process each month, but it sheds inside the abdomen rather than as menstrual blood. The tissue remains cause irritation, and develop into scar tissue that can lead to adhesions causing internal organs to stick together.
The reason we look to use at hormone/contraceptive therapy to treat endometriosis is because hormone levels influence endometrial tissue growth. The average menstrual cycle is 28 days, but it can range from 24 to 35 days in some women.
A woman’s menstrual cycle consists of three phases:
- Follicular – the first half of the cycle, commencing with the start of menses
- Ovulatory – ovulation occurs between the 12th and 16th days
- Luteal – the second half of the cycle
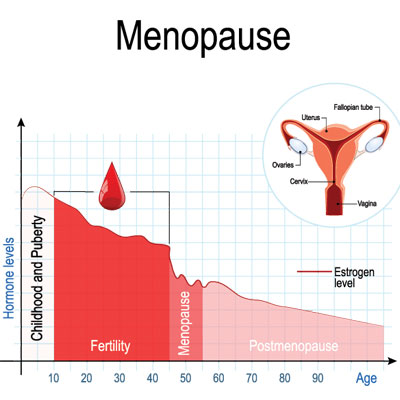
On the first day of a menstrual cycle, progesterone and estrogen levels are low. A woman will experience her first day of bleeding as the uterine lining begins to break down. The hypothalamus senses these low levels and secretes gonadotropin-releasing hormone (GnRH) to the pituitary gland. In turn, the pituitary produces follicle-stimulating hormone (FSH) and luteinizing hormone (LH) which enter the bloodstream and head to the ovaries.
FSH influences the maturation of the follicle that contains an egg. Estrogen production increases to prepare the uterus for conception and implantation by increasing the uterine lining. At the time of ovulation, elevated estrogen levels boost LH production to promote the egg release from the follicle. Both estrogen and progesterone levels increase during the surge of LH and ovulation.
Once the egg release occurs, the ruptured follicle closes and forms the corpus luteum which secretes progesterone to finish preparing the uterus for pregnancy. Progesterone helps control the uterine lining build up and maintain it during pregnancy. Estrogen levels remain high, but decrease overall. If no egg fertilization occurs, these two hormone levels drop as the corpus luteum degenerates, and menstruation begins – typically around day 28. Menstruation is the shedding of the top layers of the uterine lining.
Testosterone is the final hormone involved in the process. Its function helps boost sexual arousal and libido, especially during the time in a woman’s period when her progesterone levels are low. Elevated testosterone levels may actually suppress ovulation. Low testosterone may lead to fatigue and loss of muscle. Testosterone is also the source hormone for estrogen, just as progesterone is for testosterone. One hormonal imbalance can lead to another.
When one hormone is dominant over the others, it can lead to problems.
Women who have estrogen dominance may exhibit the following symptoms:
- Anger, mood swings, irritability
- Fluid retention
- Heavy, painful periods
- Sore or tender breasts
Progesterone dominance can cause emotional upheaval in the following ways:
- Weepy feeling and highly emotional
- Overwhelming fatigue
- Sudden lack of self-confidence
- Spots on the skin
Testosterone dominance is often associated with polycystic ovarian syndrome (PCOS). Its other symptoms may include:
- Adult acne
- Increased hair growth, especially on the face and body
- Weight gain due to increased insulin production
Symptoms of Endometriosis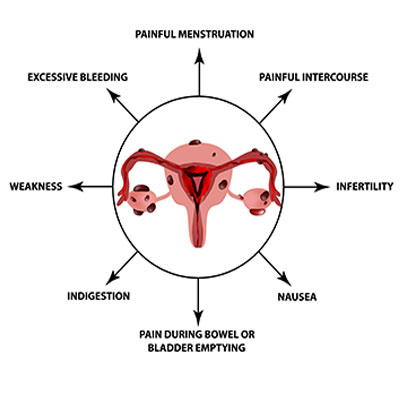
The most common symptoms of endometriosis include:
- Pain in the abdomen, lower back, and the pelvic area about a week before the onset of menstruation
- Severe cramping during menstruation
- Sexual intercourse pain – during and after
- Infertility
- Heavy bleeding during periods
- Depression
- Bleeding between periods
- Painful urination or bowel movements
- Lack of energy
- Chronic pelvic pain
Types of Hormone Therapy Used to Treat Endometriosis
There are various types of hormone treatments for endometriosis. Depending on the severity of the situation, as well as your symptoms, the doctor may prescribe any of the following treatments:
- Gonadotropin-releasing hormone (GnRH) agonists or antagonists – these medications block FSH and LH from stimulating estrogen production. Unfortunately, some women find that the prevention of menstruation from these hormones can cause menopausal symptoms. Low dose estrogen or progesterone used with the GnRH agonists and antagonists can reduce those symptoms. With this treatment, endometrial tissue begins to shrink. When the treatment ends, the periods and ability to become pregnant will return.
- Hormonal contraceptives – all forms of birth control, including pills, implants, shots, patches, and vaginal rings help control hormone levels. Menstrual flow becomes lighter and shorter in duration. Hormone treatment may help reduce endometrial pain. Contraceptive treatment consists of a combination of estrogen and progestin.
- Progestin therapy – progesterone by itself may be given to women who cannot take estrogen due to risk factors. Intrauterine devices (IUD), implants, or pills are available options. We recommend using natural progesterone rather than synthetic progestin as it is a safer treatment.
- Aromatase inhibitors – these medications reduce the conversion of testosterone into estradiol, the primary form of estrogen in the body.
The following hormone therapy for endometriosis side effects are possible:
- Breakthrough bleeding or spotting
- Mood changes
- Weight gain
- Headaches
- Nausea
- Bloating
- Breast tenderness
- Skin irritation from patches
- Vaginal irritation from vaginal rings
- Thinning hair
- Depression
- Bone density loss from progestin
- IUD may cause internal problems
Hormone therapy for endometriosis comes in many forms, giving doctors numerous options to try for the best results.
Surgical Treatment Options for Endometriosis
The word “surgery” is frightening to many people, especially for women who may be concerned about fertility. However, that should not stop you from looking at surgical options, especially if hormone therapy for endometriosis does not work.
There are two different types of surgical options, including:
- Laparoscopy: either a laser or thermal energy burns and destroys the endometriotic lesions during a day surgery procedure. Recovery time is very quick, and this option improves conception chances.
- Laparotomy: when endometriosis is more severe, a woman may require open abdominal surgery. Recovery time is longer, and the surgery may include removal of the uterus and possibly the ovaries. In extreme cases, parts of the bowel or bladder may require removal if affected. This procedure is not common.
You may also require hormonal therapy after endometriosis surgery if you have a laparoscopy to help reduce the risk of it returning. The only way to cure endometriosis is through the removal of the uterus and ovaries. However, with treatment, that is not necessary for most instances. Treating the symptoms and decreasing the cause is often all that is needed.
Other Non-Hormonal Treatments for Endometriosis
In addition to surgery and hormone treatments for endometriosis, doctors may treat the symptoms with over-the-counter pain medications. Ibuprofen is a good option for many women, as is acetaminophen or naproxen. In severe cases, a stronger prescription pain medication such as codeine may be necessary.
Alternative medication is another option to consider. Some women find relief with the following treatments:
- Acupuncture, which can help improve blood flow.
- Hot water bottle or heating pad to the abdomen
- Soaking in a hot bath to relax the pelvic muscles
- Turmeric capsules might help reduce estrogen levels and decrease inflammation
- Dietary changes such as reducing intake of gluten, dairy, sugar, red meat, and processed foods might help reduce symptoms
- Rest, including lying on the side and pulling your knees up to your chest might relieve pain
- Light exercise and stretching can help lower estrogen levels and release feel-good endorphins
- Herbal supplements – omega-3 fatty acids may help decrease inflammation
When to Try Hormone Therapy for Endometriosis
The use of hormone replacement therapy for endometriosis is the first line of treatment. Surgery is the last method when other options have failed. Turning to hormonal treatments is the obvious choice as hormones are responsible for overgrowth of endometrial tissue. For more information on hormone therapy for endometriosis, please contact our hormone clinic for a free consultation.
Hormone therapy is extremely effective at reducing the symptoms of endometriosis.
- Claudia Tosti, Antonella Biscione, MD, Giuseppe Morgante, MD, Giuseppe Bifulco, MD, Stefano Luisi, MD, PhD, Felice Petraglia, MD
- Ryan Marquardt, BS, Tae Hoon Kim, PhD, Jung-Ho Shin, Jae-Wook Jeong, PhD
- Pietro Litta, MD, PhD, Luigi Nappi, Mirian Agus, MD, PhD, Irene Melis, Gian Benedetto Melis, Stefano Angioni
- A.A. Gheorghisan-Galateanu, M.L. Gheorghiu
- Helena Malvezzi, Eliana Blini Marengo, Sérgio Podgaec & Carla de Azevedo Piccinato
Hormonal therapy for endometriosis: from molecular research to bedside
Progesterone and Estrogen Signaling in the Endometrium: What Goes Wrong in Endometriosis?
Sexual Function in Women with Deep Endometriosis: Correlation with Quality of Life, Intensity of Pain, Depression, Anxiety, and Body Image
Hormonal Therapy in Women of Reproductive Age With Endometriosis: An Update
Endometriosis: current challenges in modeling a multifactorial disease of unknown etiology