Contents
You may be more familiar with corticotropin hormone by one of its other names – adrenocorticotropic hormone, adrenocorticotropin, or ACTH. You may also see it spelled as corticotrophin hormone in some places.
No matter which name you use, they all point to the same polypeptide tropic hormone produced by the anterior pituitary gland.
Before we get into the body’s natural use and Trusted sourceCorticotrophin-releasing hormoneYou and Your HormonesGo to sourcefunction of corticotropin hormone, we want to discuss its use as a medication and diagnostic agent.
As a medication, corticotropin is called tetracosactide, tetracosacrtin, cosyntropin, and as an acetate ester called either tetracosactide acetate or tetracosactrin acetate. These medications contain the first 24 amino acids of ACTH (out of the total 39) yet continue to retain the full function of the original peptide. Tetracosactide stimulates cortisol release from the adrenal glands.
Corticotropin used as a medication treats epileptic spasms in infants and the following conditions in adults:
- Skin conditions – severe erythema multiforme, Stevens-Johnson syndrome
- Sarcoidosis in the lungs
- Acute exacerbations or maintenance therapy for systemic dermatomyositis and systemic lupus erythematosus
- Edema in specific nephrotic syndromes
- Eye conditions such as optic neuritis, diffuse posterior uveitis, iridocyclitis, choroiditis, iritis, chorioretinitis, keratitis, and anterior segment inflammation
- Acute episodes of ankylosing spondylitis, rheumatoid arthritis, and psoriatic arthritis
- Acute exacerbations of multiple sclerosis
- Serum sickness
As a diagnostic agent, tetracosactide is used to assess adrenal gland function during the Trusted sourceACTH stimulation testMedline PlusGo to sourceACTH stimulation test . One purpose of this test is to diagnose Addison’s disease.
In this report, we will discuss the following topics:
- The function of pituitary-secreted corticotropin hormone
- The regulatory process of corticotropin production
- What happens when corticotropin hormone levels are too low
- What happens when corticotropin hormone levels are too high
- How to test corticotropin levels
- The best ways to balance ACTH levels in the body
To define corticotropin hormone, also called ACTH, one could say that it is both a naturally occurring hormone as well as a medication and diagnostic agent.
What Is Corticotropin Hormone
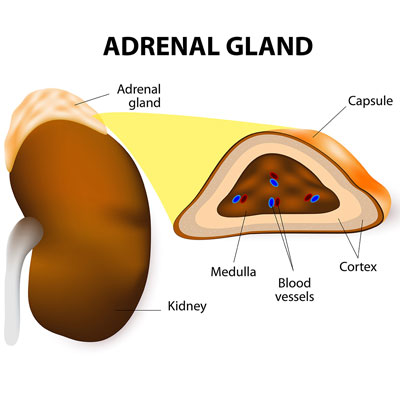
The primary corticotropin hormone function is the regulation of activity in the cortex (outer region) of the adrenal glands. ACTH is the stimulator of the adrenal cortex. Included in that function is the release of cortisol and androgen hormones from the adrenals. Cortisol release is also influenced by circadian rhythms, which is why its highest levels are in the morning. That is one of the reasons hormone specialists require blood specimen collection first thing in the morning for diagnostic testing. More on that later.
Corticotropin hormone works directly on G protein-coupled receptors found on extracellular membranes of the zona reticularis and zona fasciculata of the adrenal cortex. When activation of the G-couple receptors occurs, adenylyl cyclase is activated to increase cAMP production.
ACTH also supports immune functions and glucose metabolism.
Androgen release is an important function of corticotropin hormone. Aside from the testes and the ovaries, the adrenals also produce the androgen steroid hormones DHEA, testosterone, and estrogen. In fact, for women in menopause who no longer have ovarian hormone secretion, the adrenals are crucial for supplying these hormones.
Corticotropin hormone regulates adrenal gland production of cortisol and some androgen hormones.
What Regulates Corticotropin Hormone
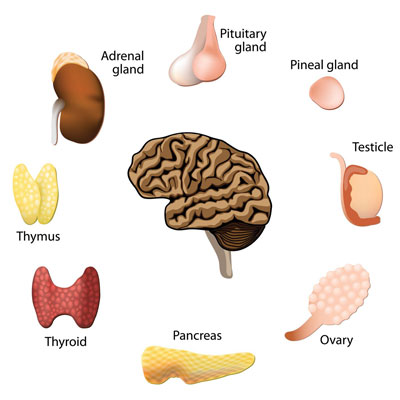
The production of ACTH is regulated by corticotrophin-releasing hormone (CRH) Trusted sourceHypothalamus OverviewHealthlineGo to sourcesecreted by the hypothalamus . Once CRH enters the anterior pituitary gland, it interacts with the corticotroph cells which release corticotropin hormone into the bloodstream. The corticotrophs make up about 10 percent of the anterior pituitary gland.
Corticotroph cells synthesize a large glycoprotein prohormone molecule by the name of proopiomelanocortin or POMC for short. The POMC molecule splits into various biologically active peptides once they are discharged from the corticotrophs. ACTH is one of the peptides.
The secretion process for ACTH is part of the hypothalamic-pituitary-adrenal (HPA) axis. The hypothalamus is the body’s regulator of many hormones. It senses various hormone levels in the bloodstream and decides which hormones to send to the pituitary gland. Following that response, the pituitary then secretes other hormones which head to various parts of the body to carry out their functions.
If ACTH levels in the bloodstream are low, the hypothalamus will sense that and send CRH to the pituitary gland. Then, corticotropin-releasing hormone function takes over and stimulates the corticotrophs into action. In return, ACTH leaves the pituitary gland and heads to the adrenal gland receptors to stimulate cortisol production. As cortisol blood levels rise, CRH secretion from the hypothalamus slows down. That action decreases the release of corticotropin hormone from the pituitary gland.
Stress is an activator of ACTH production, which is why cortisol is called the stress hormone.
Corticotropin hormone release is part of the HPA axis that begins with the hypothalamus sensing how much cortisol is in the bloodstream.
What Happens If You Have Low Corticotropin Hormone?
Hormonal imbalance can have many effects on the body, depending on which hormone is involved.
When dealing with a corticotropin hormone deficiency, low ACTH levels may be caused by the following:
- Hypopituitarism – reduced pituitary gland functions also called pituitary insufficiency, which can be due to the following:
- a pituitary adenoma (a non-cancerous tumor of the pituitary gland) that destroys the gland
- pituitary apoplexy – a sudden hemorrhage into an adenoma resulting in an immediate loss of corticotrophin
- Cushing’s syndrome – related to either an adrenal tumor or steroid medication use
- Addison disease – autoimmune destruction of all three adrenal cortex layers
- The aftermath of radiation therapy to the brain or pituitary gland surgery
- Congenital due to specific chromosomal issues
A deficiency of corticotropin hormone can occur as part of a multiple pituitary hormone deficiency syndrome called panhypopituitarism. It can also be a result of an isolated deficiency.
Symptoms of ACTH deficiency include:
- Lack of appetite
- Anorexia
- Weight loss
- Nausea
- Vomiting
- Weakness
- Low blood pressure
- Low blood sugar
- Dilutional hyponatremia (low blood sodium levels)
Low corticotrophin hormone levels could be caused by a tumor or problems with the pituitary or adrenal glands.
What Happens If You Have High Corticotropin Hormone
Elevated corticotropin hormone levels typically lead to increased cortisol secretion. When that happens, the production of testosterone and growth hormone tends to decline as cortisol is an antagonist of those hormones. Elevated cortisol levels often cause insomnia as the brain and body remain on high alert well into the evening hours.
High corticotropin hormone levels may be caused by the following:
- Adrenal insufficiency which can be due to Addison’s disease
- Congenital adrenal hyperplasia – a genetic disorder associated with inadequate production of aldosterone, cortisol, or both hormones
- Cushing’s disease – caused by an adenoma, a non-cancerous tumor of the pituitary gland (Cushing’s disease is only one potential cause of Cushing’s syndrome)
- An ectopic ACTH tumor outside of the pituitary gland that produces corticotropin hormone
Another elevated corticotropin hormone effect that could occur is hyper-pigmentation due to other chemical compounds secreted along with ACTH.
Symptoms of Cushing disease include:
- Round, full, red face (moon face)
- Upper body weight gain along with thin arms and legs
- Acne
- Skin infections
- Easily bruised skin
- Purple stretch marks on the thighs, abdomen, breasts, and upper arms
- Bone pain
- Backaches
- Weakened bones
- Fat collection between the shoulders (buffalo hump)
- Weakened muscles
- Headaches
- Fatigue
- High blood pressure
- Frequent infections
- Diabetes
- Depression
- Anxiety
- Mood or behavior changes
- Men – erectile dysfunction, low libido
- Women – irregular menstrual cycle, increased hair on face, chest, neck, thighs, and abdomen
It is essential to treat Cushing disease as it can lead to severe illness or even death if left untreated. Even after a tumor is removed, it could grow back, so continued monitoring is necessary. Complications can include diabetes, kidney stones, compression fractures in the spine, and more.
Elevated corticotropin hormone levels could be a sign of Cushing disease, which can lead to severe illness if not treated.
How Do You Test Corticotropin Hormone
The corticotropin hormone test (or ACTH test) measures the levels of not only ACTH but also cortisol in the bloodstream.
Testing these levels can help a hormone doctor detect conditions such as:
- High or low cortisol levels
- Pituitary, hypothalamic, or adrenal malfunction
- Tumor of the adrenal gland, pituitary gland, or hypothalamus
The corticotropin hormone test is done first thing in the morning when cortisol and ACTH levels are at their highest point. It is vital that you do not consume anything by mouth after midnight before the test.
An ACTH stimulation test measures serum cortisol levels before and after the administration of exogenous ACTH.
If you take steroids, you will need to stop taking them for the 48 hours preceding your blood test. Do not exercise within a 12-hour time frame before the blood sample collection. Try to avoid stress during the period, as well. Get a good night’s sleep if possible the night before the test.
Normal adult ACTH levels are between 10 and 50 pg/mL at 8 am although other labs may use a 6 to 76 or 7.2 to 63.3 pg/mL range as normal.
Your hormone specialist may also order a 24-hour urine cortisol collection or cortisol saliva test. If there is a concern over a tumor, you will likely undergo a brain MRI.
It is vital to contact a hormone specialist for blood analysis is corticotropin hormone imbalance is suspected.
How Do You Balance Corticotropin Hormone?
If you have low corticotropin hormone levels, the doctor may treat you with cortisol therapy to help normalize cortisol levels. If a tumor is the cause, surgery and/or radiation treatment may be necessary.
If you have an increased corticotrophin level due to Cushing disease brought about by a tumor, then, again, surgery and/or radiation therapy may be required. If treatment does not stop excess cortisol production, then medication may be necessary to prevent the body from secreting cortisol into the bloodstream.
Following surgery, if the pituitary gland is intact, it may take some time to return to normal hormone production. During that time, supplemental hormone replacement therapy may be necessary for any impacted hormone levels.
Radiation therapy is often used when the entire tumor is not completely removed.
For questions about corticotropin hormone or any other hormonal imbalance, please contact HGH Doctor hormone clinic for a free and confidential consultation by phone.
- Heinrich M. Schulte, MD, George Chrousos, MD, ScD, MACE, MACP, FRCP, P C Avgerinos, Edward H. Oldfield, MD, Philip Gold, MD, Gordon B. Cutler, Lynn D. Loriaux, MD, PhD
- Catherine Rivier, PhD, Michael Brownstein, MD, PhD, Joachim Spiess, Jean Rivier, Dr. Wylie Vale
- Dr. Rainer Rupprecht, Dr. Klaus-Peter Lesch, Ulrich Müller-Sedgwick, MD, PhD, Georg Beck, Dr. Helmut Beckmann, Dr. Heinrich M. Schulte
- Yizhou Jiang, Tangming Peng, Uma Gaur, Marta Silva, Peter Little, Zhong Chen, Wei Qiu, Yandong Zhang and Wenhua Zheng
- A. Slominski
- Dr. Sanchari Sinha Dutta, Ph.D. Reviewed by Dr. Jennifer Logan, MD, MPH
The Corticotropin-Releasing Hormone Stimulation Test:A Possible Aid in the Evaluation of Patients with Adrenal Insufficiency
In Vivo Corticotropin-Releasing Factor-Induced Secretion of Adrenocorticotropin, Endorphin, and Corticosterone
Blunted adrenocorticotropin but normal beta-endorphin release after human corticotropin-releasing hormone administration in depression
Role of Corticotropin Releasing Factor in the Neuroimmune Mechanisms of Depression: Examination of Current Pharmaceutical and Herbal Therapies
On the role of the corticotropin-releasing hormone signalling system in the aetiology of inflammatory skin disorders
Corticotropin-Releasing Hormone (CRH)