Contents
- Hysterectomy and Oophorectomy Effects on Hormone Secretion
- Surgical Menopause and Hormone Replacement Therapy
- Is Hormone Replacement Therapy Necessary After Hysterectomy?
- How to Determine What Type of Hormone Replacement Therapy is Best
- Menopausal Symptoms After Hysterectomy
- Pros and Cons of Hormone Replacement Therapy After Hysterectomy
- Risks of Hormone Replacement Therapy after a Hysterectomy
- How Long Do I Have to Take HRT After a Hysterectomy?
- What Happens if You Don’t Take Estrogen After a Hysterectomy?
- What Does the Research Say About Hysterectomy and Hormone Replacement?
Most women can benefit from hormone replacement surgery after having a hysterectomy.
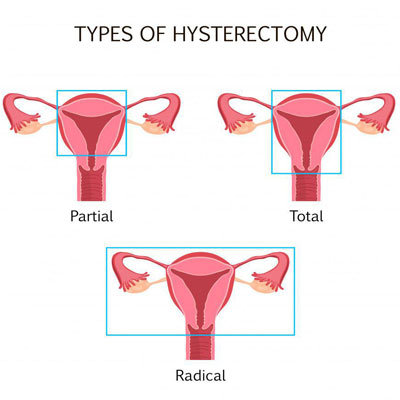
Doctors perform an average of 500,000 hysterectomies a year in the US. These hysterectomies can be partial, total, or radical, depending on what structures are removed.
A hysterectomy often will also involve the surgical removal of the ovaries or oophorectomy. This will result in a fundamental decrease in estrogen, creating a condition that doctors refer to as “surgical menopause.”
In many cases, hormone replacement therapy after surgery is an effective way to counteract the supply of estrogen women lose after a hysterectomy.
A hysterectomy is a surgical procedure that removes a woman’s uterus and often her ovaries as well.
Hysterectomy and Oophorectomy Effects on Hormone Secretion
A hysterectomy does not always affect hormone levels. What does occur is that a woman will stop having monthly periods once her uterus is removed. Women who have a hysterectomy but retain their ovaries will usually not experience signs of menopause for many years after surgery. Others may start to get hot flashes and other menopause symptoms a short time after the surgery. The reason why a woman might need hormone replacement therapy after hysterectomy is due to reduced blood flow to the ovaries following the uterine removal. If the ovaries decrease their hormonal production, the symptoms of menopause may appear. The decline in hormone secretion here is not the same as with oophorectomy or surgical removal of the ovaries.
The ovaries are the manufacturers of progesterone, testosterone, and estrogen. When a doctor performs an oophorectomy, he is removing the primary source of hormone production for these chemical messengers. Although a small amount of these hormones will still come from the adrenal glands, the loss of the ovaries often sends women into what is called “surgical menopause.” This condition comes on rather quickly since hormone levels rapidly decline.
Surgical Menopause and Hormone Replacement Therapy
A complete hysterectomy, including oophorectomy, has significant hormonal implications. Regardless of a woman’s age, if the ovaries are removed during a hysterectomy, it creates a condition known as “surgical menopause.” Since the ovaries are the primary producers of estrogen, any surgical procedure that removes the ovaries in premenopausal women will result in surgical menopause.
Estrogen plays a key role throughout a woman’s life. It is essential for:
- Sex drive and sexual satisfaction
- Brain health and cognition
- Healthy skin and bones
- Heart health
- And more.
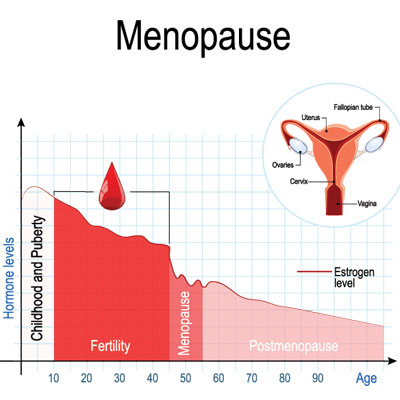
When a woman reaches her last menstrual period, usually around the age of 50, she can start feeling the well-known symptoms of menopause – mood swings, night sweats, hot flashes, etc. These debilitating symptoms are a reaction to a gradual loss of estrogen before, during, and after menopause.
However, estrogen levels plummet all at once with surgical menopause. That sudden drop in estrogen can lead to menopausal symptoms that can be much more severe than during natural menopause.
When it comes to treating the symptoms of natural menopause, hormone replacement therapy is a bit of an individual choice. However, HRT is highly recommended for women experiencing surgical menopause. This is especially true for women who have had to have a hysterectomy at a relatively young age.
Hysterectomy can bring on “surgical menopause.”
Is Hormone Replacement Therapy Necessary After Hysterectomy?
Surgical menopause will occur after an oophorectomy. In this case, estrogen replacement is almost always recommended.
A 2007 study discussing the decision to have HRT to post-hysterectomy patients concluded, “When a bilateral oophorectomy is performed before natural menopause, the onset of menopausal symptoms, primarily vasomotor symptoms, genital tract atrophy, and/or a decline in sexual function, is rapid, and the symptoms are more severe. Thus, the need for a decision on the use of hormone therapy is accelerated.”
In hysterectomy that does not include removal of the ovaries, surgical menopause does not occur, yet most doctors suggest that hormone replacement therapy after hysterectomy is a good idea.
Ovaries produce hormones, primarily estrogen and progesterone, that control menstrual cycles and menopause. If surgery removes a woman’s uterus, but not her ovaries, the ovaries keep making hormones but at a lower level. If you have a hysterectomy but keep your ovaries intact, you will not immediately go into surgical menopause. However, you could develop hormonal imbalances or go into menopause earlier than usual. In either case, HRT may be recommended.
How to Determine What Type of Hormone Replacement Therapy is Best
The type of hysterectomy you have will largely determine the kind of hormone replacement therapy that is best post-surgery. Your HRT will consist of estrogen and progestin or estrogen alone. Women who have both the uterus and ovaries removed will usually only get estrogen replacement therapy alone. But women who have only the ovaries removed need both estrogen and progestin. That’s because estrogen alone can increase the risk of cancer in the uterus. Adding progestin removes this risk.
Menopausal Symptoms After Hysterectomy
The menopausal symptoms a woman will experience after hysterectomy will echo those of natural menopause including:
- Sudden and more severe onset of menopausal symptoms: in particular; hot flushes, night sweats, and vaginal dryness
- Loss of bone density and increased risk of osteoporosis and fracture
- Impaired sexual function due to reduced desire and discomfort from vaginal dryness
- Reduced sex drive (libido) associated with loss of ovarian testosterone production
- Loss of fertility
- Increased risk of cardiovascular (heart) disease
Pros and Cons of Hormone Replacement Therapy After Hysterectomy
Hormone replacement therapy is generally regarded as safe. It is recommended for women, especially younger women, after hysterectomy. However, as with all prescription medications or medical procedures, it is not entirely risk-free.
The decision to have HRT after hysterectomy surgery requires careful consideration and will be made between you and your doctor. However, for most patients, the “pros” outweigh the “cons.”
When properly prescribed and well-managed by qualified physicians like ours, the risks of HRT are actually quite small for any given patient. A hysterectomy will only be performed if it is a necessary medical procedure. Yet, it can be very emotionally traumatizing for a woman. That emotional distress will only be made worse by the early onset of menopausal symptoms. HRT post-surgery can help a woman to maintain the active, satisfying life she deserves.
Benefits of Hormone Replacement Therapy after Hysterectomy
When estrogen levels drop immediately post-hysterectomy, a woman’s hormonal balance is thrown into total confusion. She can experience the sudden and severe onset of menopausal symptoms such as:
- Fatigue
- Lack of sex drive
- Hot flashes
- Night sweats
- Mood swings
- Painful intercourse and vaginal dryness
- Joint pain
- Impaired memory, lack of focus, and other cognitive difficulties
- Weakened immune function
- Weight gain
- Increases anxiety and depression
Post-surgical hormone replacement therapy can reduce or even eliminate most, if not all, of these symptoms.
As in women taking HRT for natural menopause, there can be additional benefits for women undergoing hormone replacement for surgical menopause. HRT may also reduce the risk of diabetes, heart disease, and osteoporosis.
The symptoms of surgical menopause can be treated with hormone replacement therapy.
Risks of Hormone Replacement Therapy after a Hysterectomy
Hormone replacement therapy is generally regarded as a safe and effective treatment for menopausal symptoms, whether they are brought on by natural menopause or after a hysterectomy. However, HRT, like any drug or medical procedure it has some risk.
Some of the potential side effects of hormone replacement after a hysterectomy include:
- Breast tenderness
- Bloating
- Upset stomach
- Swelling in other parts of the body
- Leg cramps
- Headaches
- Indigestion
- Vaginal bleeding
In addition, hormone replacement therapy may increase the risk of health problems in a small number of women. This increase in risk depends on your age, past medical condition, and family history. Talk with your doctor about these risks. HRT post-hysterectomy may increase your risk of:
- Stroke.
- Blood clots.
- Gallstones.
You should probably not have HRT:
- You have unexplained vaginal bleeding.
- You have liver disease or other problems with your liver.
- You have breast cancer, ovarian cancer, uterine cancer, or blood clots, or have had a stroke.
How Long Do I Have to Take HRT After a Hysterectomy?
HRT is recommended for all women who undergo surgical menopause under the age of 45, provided they do not have contraindications to hormone replacement therapy. If you’re able to have HRT and both of your ovaries have been removed, it’s important to continue with the treatment until you reach the normal age for menopause (51 is the average age). You may choose to continue HRT at that time.
What Happens if You Don’t Take Estrogen After a Hysterectomy?
Estrogen plays a key role throughout the body. It affects the brain, the bones, the skin, the heart, the blood vessels, and more. While estrogen levels lower gradually during natural menopause, they plummet with surgical menopause. That sudden drop in estrogen can lead to menopausal symptoms that can be quite severe.
Among other potential negative consequences, if you do not take estrogen after hysterectomy, you are at risk for weak bones later in life, which can lead to osteoporosis.
What Does the Research Say About Hysterectomy and Hormone Replacement?
There have been many studies that validate the use of hormone replacement in women that have had hysterectomy along with oophorectomy.
The most recent and definitive, such study found that in young women who had bilateral oophorectomy prior to menopause, “Without hormone replacement therapy most of these women develop severe symptoms of estrogen deficiency and are at increased risk for osteoporosis, cardiovascular disease, cognitive decline, dementia, and the associated increases in morbidity and mortality.” This study concluded that “Timely and effective HRT for women who will experience surgical primary ovarian insufficiency is clearly indicated.”
FAQ
- Dr. Arthur F Haney, MD, Robert A Wild, MD, MPH, PhD
- Sue Furness, Jane Marjoribanks, Prof. Martha Hickey, Dr. Helen Roberts, Professor Cindy Margaret Farquhar, CNZM, FRNZ, MBChB, DipObMedGyn, MD, FRCOG, FRANZCOG, CREI, MPH, Anne Lethaby
- Ronald K. Ross, Annlia Paganini Hill, PhD, Peggy Wan, Malcolm Pike, PhD
- By Brendan Ayres, Reviewed by Kenneth Varano D.O.
Options for hormone therapy in women who have had a hysterectomy
Hormone therapy in postmenopausal women and risk of endometrial hyperplasia
Effect of Hormone Replacement Therapy on Breast Cancer Risk: Estrogen Versus Estrogen Plus Progestin
Hormone Replacement Therapy After Hysterectomy