Contents

Trusted sourceMayo ClinicMuscular dystrophyGo to sourceMuscular dystrophy is the name for a group of diseases that lead to the loss of muscle mass and progressive weakening of the body. Abnormal gene mutations interfere with the formation of healthy muscle by decreasing or inhibiting protein production. Some types of MD begin during childhood, while others surface many years later during adulthood.
MD can result in scoliosis, contractures, respiratory impairment, feeding and swallowing difficulties, and metabolic alterations.
Although there are approximately 30 different types, here are the most common forms of muscular dystrophy:
- Duchenne muscular dystrophy (DMD) is the most common, affecting boys more commonly than girls. Symptoms appear early in childhood and can affect walking, running, jumping, rising, and learning.
- Becker muscular dystrophy (BMD) is the next most common, but its symptoms typically do not begin until the teenage years, or later. Symptoms are similar to DMD, but progress more slowly and are generally milder.
- Congenital muscular dystrophy affects girls and boys and is apparent either at birth or by age 2. This disease may progress slowly with mild disability or rapidly with severe impairment.
- Limb-girdle MD (calpainopathy) affects the hip and shoulder muscles first, often causing difficulty with foot lifting. Childhood or teenage onset is most common.
- Facioscapulohumeral (FSHD) occurs most often during teenage years but can also begin in childhood or adulthood – typically up to age 40. FSHD affects the face and shoulder muscles, sometimes causing the shoulder blades to stick out upon arm raising.
- Steinert’s or myotonic MD is the most common adult-onset form (one in 8000 individuals) that often begins in the neck or facial muscles.
One reason to look for a connection between HGH and muscular dystrophy is that human growth hormone influences muscle growth and structure. Studies question whether HGH can strengthen the muscles of people with MD to improve physical function and movement.
The current study of HGH treatments for muscular dystrophy focuses on FSHD and includes the use of testosterone enanthate as well as HGH therapy. Ongoing research of subjects at the University of Rochester Medical Center in Rochester, NY, looks at how 24 weeks of treatment can help improve symptoms of FSHD in males. We look forward to hearing about the results of this study that began in 2017 in the future.
In one study of a patient with calpainopathy, daily treatments of HGH continued for four and a half years, with one six-month pause. Muscle group strength improved during treatment and deteriorated during the six months of no HGH therapy. Once treatment began again, the improvements continued.
Because muscular dystrophy affects the muscles, movement, and strength, there is a need for increased research into the possible benefits of HGH for MD.
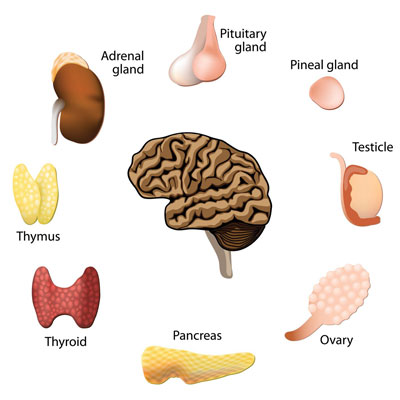
Endocrine Alterations in Muscular Dystrophy
Before 2009, there were no substantial discussions on the hormones involved with muscular dystrophy. However, in October 2009, the first conference was held to discuss the endocrine aspects of DMD.
Boys with Duchenne muscular dystrophy often experience short stature, delayed puberty, osteoporosis, and obesity, among other issues. The conference looked at these concerns, as well as the impact of Trusted sourceHealth LineCorticosteroids: What Are They?Go to sourcecorticosteroids on the body.
The use of corticosteroids for MD is crucial, as it can help slow disease progression and improve pulmonary and cardiac functions. However, the impact on endocrine function is significant. In men with MD, endocrine disturbances such as infertility, low testosterone, and growth hormone deficiency are possible.
Muscular dystrophy can cause damage to the cell membrane of myocytes (muscle cells). Because skeletal muscle accounts for at least 70 percent of glucose uptake, disposal, and storage, loss of skeletal muscle due to MD can lead to insulin resistance.
The endocrine alterations that occur in boys of pubertal age with DMD can affect them emotionally, as well. They see their peers growing and developing faster than they are, which can further the depression of dealing with an ongoing medical condition, as well as impacting their quality of life. Chronic corticosteroid use can suppress growth hormone production, reducing insulin growth factor 1 levels, and impacting bone growth and strength. In one study of 39 boys with DMD, HGH treatments for muscular dystrophy showed improved linear growth and BMI (body mass index).
Testosterone levels are another area of concern, as they are also influenced by HGH production. Boys with DMD may also experience testosterone deficiency which can impact bone density and muscle growth. While testosterone therapy may prove beneficial, given to youth without the addition of HGH could result in bone age advancement and epiphyseal fusion, compromising full adult height achievement. It is essential to look at all endocrine issues when contemplating HGH and possibly testosterone treatment in boys with muscular dystrophy.
Endocrine abnormalities in adult myotonic dystrophy can also lead to testicular atrophy in males (besides infertility and low testosterone). Females with adult MD can also suffer from reduced fertility, as well as an increased risk of spontaneous abortion and early menopause.
Altered hormone levels in patients with muscular dystrophy could influence fertility, leading to infertility in men and women.
HGH Influence on Metabolic Alterations in Muscular Dystrophy
As we continue to explore the possibility of using HGH for muscular dystrophy, we turn to metabolic alterations on the body. Skeletal muscle protection is crucial, not just for movement, but also for its role in glucose metabolism. Loss of muscle can lead to Trusted sourceMedline PlusMetabolic DisruptionsGo to sourcemetabolic disruptions such as weight gain (obesity) and insulin resistance. These problems can further the risks associated with cardiovascular disease. Obesity is a significant problem for adults with myotonic dystrophy. Because lung capacity also declines, it can make it harder to engage in physical activity, which is vital to protect against fat retention.
The potential use of HGH treatments for muscular dystrophy can help improve insulin sensitivity, glucose uptake by the cells, and metabolic functions for lipolysis. Insulin resistance is the primary cause of glucose intolerance in adults with myotonic dystrophy type 1. Abnormal insulin secretion is another possible issue. Losing weight is an excellent way to increase HGH and testosterone production. At the same time, HGH improves muscle mass and strength, two areas that can help enhance mobility and physical performance.
Physical activity is critical for bone growth, both during childhood and adulthood. For adults, working out with weights (resistance training) can help support bone density and reduce the risk of osteoporosis. Because growth hormone deficiency causes muscle weakness and fatigue, it can make it difficult to exercise. HGH therapy can help improve energy, sleep, muscle, and bone strength, along with cardiac output for increased exercise ability.
Another potential area of improvement is in the cardiovascular health of patients with BMD and DMD. One study looked at the use of HGH therapy as compared to a placebo for three months. In patients who received recombinant human growth hormone treatment, left ventricular mass increased as follows:
- 16% in BMD patients
- 29% in DMD patients
The results also show left ventricular end-systolic stress declined 13% and 33% in BMD and DMD patients, respectively. At the same time, brain natriuretic peptide levels decreased by 40%.
HGH treatments for muscular dystrophy may provide benefits for muscle mass, bone density, fertility, cardiovascular health, and glucose uptake.
Can HGH Treatment Help Muscular Dystrophy?
One of the common treatments for muscular dystrophy is corticosteroids, which can help maintain muscle strength while delaying MD progression. However, corticosteroids are associated with weakened bones, osteoporosis risk, and weight gain. The potential use of HGH treatments for muscular dystrophy may help support muscle tone and strength while also stimulating weight loss and increasing bone density.
The need for more research into adult muscular dystrophy and growth hormone deficiency is crucial. Back in 1981, it was reported that low growth hormone levels could be linked to adults with MD. The connection between low HGH levels and muscular dystrophy shows that there may be a communications failure in the chemical signaling in the brain.
Can HGH help muscular dystrophy symptoms in adults?
Although considerable research is necessary before any definitive answer is made, the possibility exists that HGH therapy could improve certain symptoms of adult MD. Adult and childhood-onset muscular dystrophies present in different ways. Males diagnosed with DMD as children often have short stature, which is not an issue for adults diagnosed with MD later in life. Both metabolic and endocrine manifestations are also different, as they can impact the body early in life with both DMD and BMD. By adulthood, these individuals may be limited to the use of a wheelchair.
We recommend seeking hormone testing for adults with MD to determine if any deficiencies may account for specific symptoms. Endocrine consultation may provide insight into potential treatments.
- Antonio Cittadini, Prof., Lucia Ines Comi, MD., Salvatore Longobardi, Vito Rocco Petretta, MD., Cosma Casaburi, Luigia Passamano, Bartolomeo Merola, Emanuele Durante-Mangoni, Prof., Luigi Saccà, MD., Luisa Politano, MD.
- M Zatz, Prof., physician, biologist, R T Betti, O Frota-Pessoa, physician, biologist.
- Chad R Heatwole, MD, MS-CI.
- Sung‐Hee Yoon, PhD., Marc D Grynpas, PhD., Jane Mitchell, PhD.
A preliminary randomized study of growth hormone administration in Becker and Duchenne muscular dystrophies
Treatment of Duchenne muscular dystrophy with growth hormone inhibitors
Study of Testosterone and rHGH in FSHD (STARFISH)
Growth Hormone Increases Bone Toughness and Decreases Muscle Inflammation in Glucocorticoid‐Treated Mdx Mice, Model of Duchenne Muscular Dystrophy