Low Testosterone and Cholesterol
Contents
Testosterone plays a critical role in maintaining a man’s health and vitality. Testosterone is essential for bone and muscle growth. It is also linked to sex drive and fat metabolism. That last one, the quintessential role that testosterone plays in how your body burns or stores fat, is at the root of the relationship between your testosterone level and your cholesterol level.
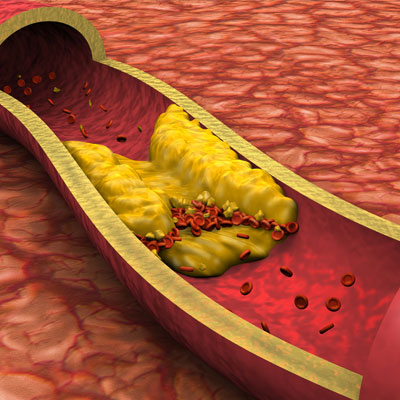
Cholesterol is a kind of fat in your blood. It serves a purpose in the growth and maintenance of certain tissues and cells. But, if you have too much of it, it can build up on the walls of your blood vessels and make them narrow. This is what is meant when we say someone has “high cholesterol.” When cholesterol builds up like that, it can make it harder for your blood to move through your body. This can lead to high blood pressure and an increased risk of heart disease.
But not all cholesterol is bad. There are two of cholesterol — LDL and HDL.
LDL cholesterol is the kind that builds up in your blood vessels, causing heart problems. LDL is often called “bad” cholesterol because it leads to this buildup of arterial plaque. HDL cholesterol is known as “good” cholesterol because it helps the liver to break down and to flush out LDL, or “bad” cholesterol.
There seems to be a link between high cholesterol and low testosterone.
Can Low Testosterone Cause High LDL?
Men with low testosterone tend to have high levels of LDL (“bad”) cholesterol in their blood. We cannot definitively say that one causes the other, but it is well-documented that the two conditions often go hand-in-hand.
We also know that as men get older, their ability to produce testosterone declines. Older men who are suffering from low testosterone are also more likely to have heart problems and high cholesterol.
Men with low testosterone tend to also have high levels of cortisol. Cortisol is called the “stress hormone.” It is released in response to stress. Cortisol is also known as a “testosterone killer.” The higher the level of cortisol in the blood, the lower the level of testosterone. High levels of cortisol in the blood are also related to high cholesterol.
Studies have shown that high levels of cortisol from long-term stress may be the mechanism behind how stress can increase cholesterol. The dynamic relationship between stress, cortisol, and low testosterone is another way that testosterone and cholesterol are linked.
How Does Low Testosterone Affect Cholesterol Metabolism?
Low testosterone, particularly age-related testosterone deficiency, slows down the metabolism and leads to increased fat storage. This can lead to obesity and related problems such as high LDL cholesterol. There are two types of cholesterol: LDL cholesterol, which is considered the “bad,” and HDL, which is the “good” cholesterol.
Too much of the bad kind, or not enough of the good kind, increases the risk that cholesterol – a waxy-like substance — will slowly build up in the inner walls of the arteries that feed the heart and brain. This increases the risk of cardiovascular disease. Because low testosterone affects your cholesterol level, men with age-related testosterone decline are at greater risk of cardiovascular disease.
Testosterone, Cholesterol, and Metabolic Syndrome

Metabolic syndrome is described as a series of medical problems that together increase your risk of heart disease, stroke, and type 2 diabetes. Most of the risk factors for developing metabolic syndrome are related to obesity. Men with low testosterone tend to be overweight. In particular, they have an excess of belly fat. Men with low testosterone tend to also have one or more of the conditions associated with metabolic syndrome, including high cholesterol.
Does Testosterone Therapy Lower Cholesterol?
Testosterone replacement therapy has many positive effects on heart health, not the least of which is lowering your levels of “bad” (LDL) cholesterol and increasing your levels of “good’ (HDL) cholesterol.
Men who are between the ages of 45 and 65 are most likely to be suffering from low levels of testosterone. These are the very same men who are most likely to be obese and/or have high cholesterol.
Testosterone replacement therapy is not seen as a “treatment” for high cholesterol. However, testosterone therapy can increase your metabolism, help you to get rid of fat, and build muscle mass, all of which could lower your cholesterol and make you less likely to have a heart attack.
Testosterone therapy is used to treat men experiencing age-related testosterone loss. One of the many benefits of testosterone therapy is increased fat metabolism and weight loss, particularly belly fat. This reduction in fat certainly can lower your cholesterol levels. Studies have found that losing as little as 5% of your body weight can lower your bad (LDL) cholesterol levels by as much as 20 points.
In addition to helping you to lose weight and lower your risk of heart attack, by lowering your cholesterol level, testosterone therapy for men can also:
- Improve your sex drive
- Provide you with increased strength and more energy
- Help you to build lean muscle (which also can lower your cholesterol)
- Improve sleep
- Improve mood
- Improve memory and cognition
What Does the Medical Research Say About Testosterone and Cholesterol?
There is research to suggest correlations between men with low testosterone and high cholesterol and, therefore, a greater risk of the development of cardiovascular disease.
A 2013 study looked at the long-term effects of testosterone and the risk for metabolic syndrome. One factor of metabolic syndrome is high cholesterol levels. The researchers followed 255 men who had low testosterone levels and symptoms of low T. At the beginning of the study, all of the participants had elevated triglycerides, and about 22% had low HDL cholesterol levels. One group received testosterone replacement therapy, while the other received a placebo.
Over the five-year study, those in the testosterone replacement group saw a “significant decrease in total cholesterol levels, LDL cholesterol levels, and triglycerides.” Also, the testosterone replacement group saw a small increase in their HDL cholesterol levels. The study was published in the International Journal of Clinical Practice.
Just as men with low testosterone seem to have higher levels of bad (LDL) cholesterol, men with normal or high testosterone levels tend to have increased levels of “good” cholesterol. One year-long study involving over 4,000 men (The Massachusetts Male Aging Study) studied the correlation between HDL cholesterol and testosterone levels. The research confirmed that men who had higher levels of HDL cholesterol also had higher levels of testosterone.
Another study of men with Type II Diabetes also drew a direct link between HDL cholesterol and testosterone levels. This study indicated that the lower HDL was, the lower testosterone was.
There definitely seems to be a correlation between healthy testosterone levels and “good” (HDL) cholesterol levels.
Now that you know a lot more about your testosterone levels and how that can impact your cholesterol levels and your risk of heart disease, why not contact us today and learn more about the many benefits of testosterone replacement therapy.
- Arthi Thirumalai MD., Katya B Rubinow MD., and Stephanie T Page MD., PhD.
- Peter Jaret, James Beckerman, MD.
- A. M. Traish PhD., A. Haider MD., G. Doros PhD., F. Saad PhD.
An update on Testosterone, HDL and cardiovascular risk in men
Long-term testosterone therapy in hypogonadal men ameliorates elements of the metabolic syndrome: an observational, long-term registry study